Case Report
“Bulls Eye For Bulls Teeth”- Endodontic Management of Taurodontism Using CBCT as A Diagnostic Tool- 2 Rare Case Reports

Sapna Sonkurla1, Manoj Mahadeo Ramugade1*, Shubha Hegde1, Gopal Tawani2
1Department of Conservative Dentistry and Endodontics, Government Dental College and Hospital, Mumbai, India
2Department of Conservative Dentistry and Endodontics, Sharad Pawar Dental College, Sawangi, Maharashtra
*Address for Correspondence: Manoj Mahadeo Ramugde, M.D.S Associate Professor, Department of Conservative Dentistry and Endodontics, Government Dental College and Hospital, Mumbai, India, Tel: 09869159131; Email: [email protected]
Dates: Submitted: 20 December 2016; Approved: 19 January 2017; Published: 20 January 2017
How to cite this article: Sonkurla S, Ramugade MM, Hegde S, Tawani G. “Bulls Eye For Bulls Teeth”- Endodontic Management of Taurodontism Using CBCT as A Diagnostic Tool- 2 Rare Case Reports. J Clin Adv Dent. 2017; 1: 005-011. DOI: 10.29328/journal.jcad.1001002
Copyright License: © 2017 Sonkurla S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Taurodontism; Bifurcation; Trifurcation; Cone Beam Computed Tomography (CBCT)
Abstract
Taurodontism is a rare dental anomaly presented with an aberration of teeth that lacks the constriction at the level of the cemento-enamel junction (CEJ). It is characterized by elongated pulp chambers and apical displacement of bifurcation or trifurcation of the roots, forming a rectangular shape. Whilst, it appears most frequently as an isolated anomaly, its association with several syndromes and abnormalities has also been reported in the literature. Although permanent molars are most commonly affected, this anomaly could also be seen in deciduous dentition, unilaterally or bilaterally, and in any combination of teeth or quadrants. These morphological anomalies pose various challenges to the dentist during their endodontic treatment. Modern diagnostic tools such as Cone beam computed tomography (CBCT), loupes and Dental operating microscopes (DOM) help in achieving better treatment outcome in such cases. The presented article elaborates diagnosis and successful management of 2 rare cases of taurodontism in permanent molars.
INTRODUCTION
Taurodontism is a rare clinical entity and can be defined as a change in tooth shape caused by the failure of Hertwig’s epithelial sheath diaphragm to invaginate at the proper horizontal level. It has a prevalence rate of 2.5 to 3.2% [1]. However a wide variation in prevalence rates have been noted in various studies owing to racial differences and variations in study methods [2]. These taurodontic teeth are usually identified on the radiograph by elongated pulp chambers and apical displacement of bifurcation or trifurcation areas of the roots. Due to this, clinically the chamber has a greater apico-occlusal height giving a false feeling of perforation and lacks the constriction at the level of CEJ giving it a rectangular shape. Thus, the distance from the bifurcation of roots to the CEJ is greater than the occluso cervical distance [3,4]. Taurodontism can occur alone, limited to one or more teeth or it can be associated with various syndromes like Down syndrome [5], Klinefelter syndrome [6], ectodermal dysplasia [7], Smith-Magenis syndrome [8], thalassaemia major [9], tricho-dento-osseous syndrome [10], cleft lip and palate [11] and Van der Woude syndrome [12]. It could be unilateral or bilateral and affects permanent teeth more frequently than the primary teeth [13].
Depending upon the bifurcation or trifurcation level i.e. based on the degree of apical displacement of the pulpal floor, taurodontism may be classified as mild, moderate and severe (Hypotaurodontism, Mesotaurodontism and Hypertaurodontism respectively) [13-15]. Later, a quantitative expedient to identify taurodontism from radiographs was suggested by Shifman and Chanannel [16]. They proposed a taurodontic index (TI) obtained by dividing the height of the pulp chamber by the distance between the occlusal end of the pulp chamber and the root apex and then multiplying the number by 100. A tooth is diagnosed with taurodontism if the index (TI) is equal to or greater than 20 [16]. This biometric method has been largely based on 2-dimensional (2D) periapical radiographs or panoramic radiographs, which may not reflect the real dimensions of all the parameters. Therefore, cone-beam computed tomographic (CBCT) imaging is recommended to aid in the diagnosis of taurodontism. Endodontic management of taurodont teeth is stated to be difficult and challenging due to the complexity in the tooth morphology. This case report presents clinical implications and successful endodontic management of two cases of taurodontism in permanent maxillary and mandibular molars.
CASE 1
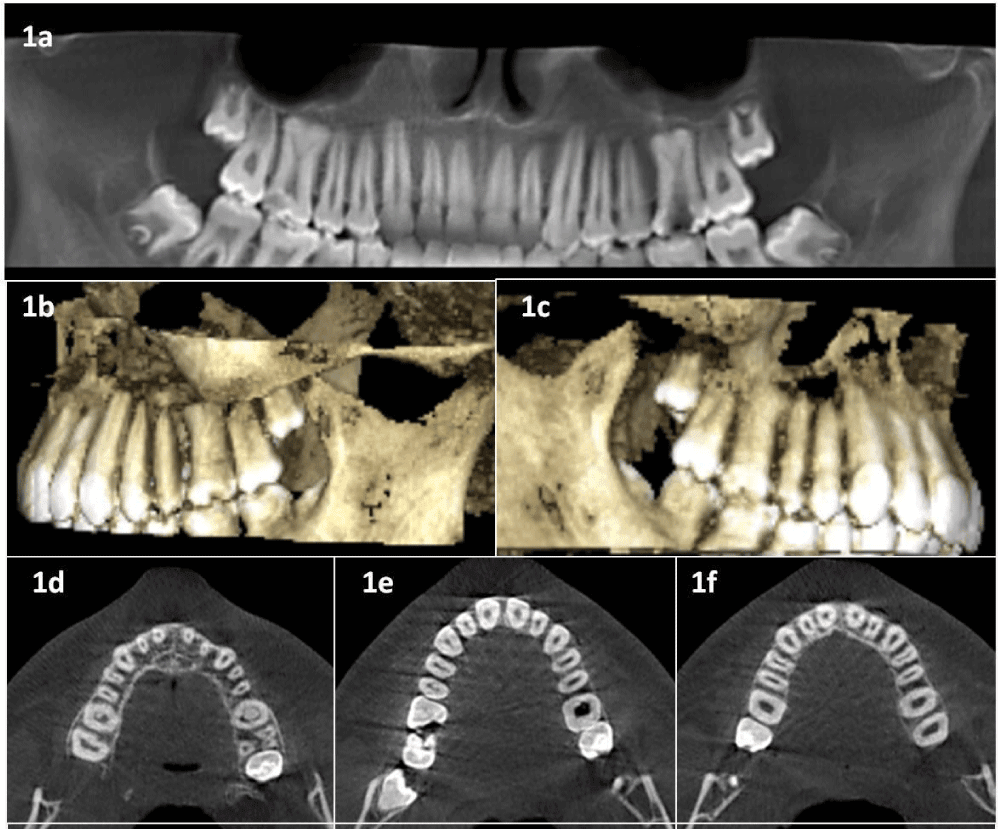
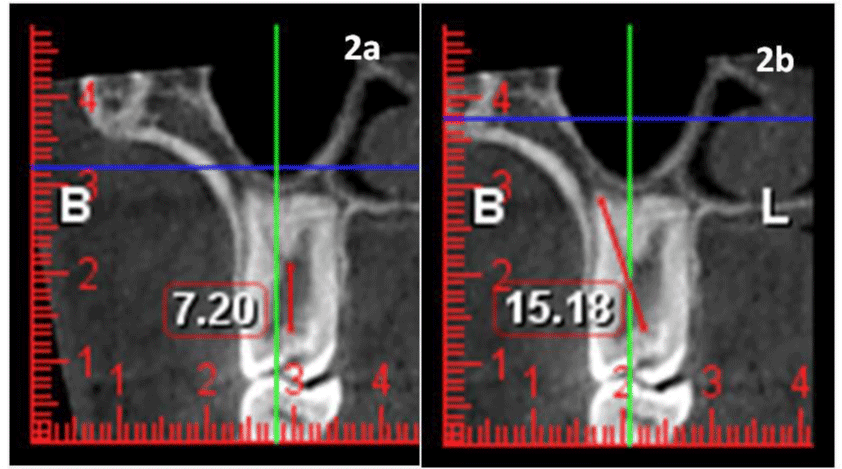
A 16-year-old healthy male patient reported to Department of Conservative dentistry and Endodontics, with a chief complaint of food lodgement in decayed maxillary molar teeth. Intraoral examination revealed usual anatomy of crowns with deep occlusal caries in tooth #16 and #26 (Universal notation system). Affected teeth were not sensitive to percussion or palpation. Vitality testing in tooth #16 and #26 showed no response to thermal and electric pulp testing indicating necrotic pulp. Intraoral periapical radiograph (IOPA) of #16 and #26 revealed occlusal radiolucency approaching pulp with a huge pulp chamber extending beyond the CEJ reaching the furcation in the apical third region. Three short roots were seen at the furcation area in the apical third suggestive of hypertaurodontism in tooth #16 and #26. To further confirm the diagnosis, modern diagnostic aid CBCT was taken (Figure 1). Using CBCT software the height of pulp chamber was measured to be 7.2 mm and that from occlusal end of pulp chamber to root apex was 15.18 mm. (Figure 2a,2b). Curiosity prompted us to take the intraoral periapical radiographs of lower molars (after getting the consent from the parents). To evaluate presence of taurodontism in the lower molars, their IOPA was advised which did not show any characteristic of taurodontism. The diagnosis of pulp necrosis with bilateral hypertaurodontism in tooth #16 and #26 was made based on the clinical, radiographic and CBCT findings.
Figure 1: CBCT images showing taurodontism in #16 and #26. a: Panoramic view 1b and 1c Lateral views of 3 dimensional rendering models. 1d, 1e and 1f : Axial section at coronal, middle and apical thirds of root.
Figure 2: The height of pulp chamber was measured to be 7.2 mm. b: distance from occlusal end of pulp chamber to root apex was 15.18 mm.
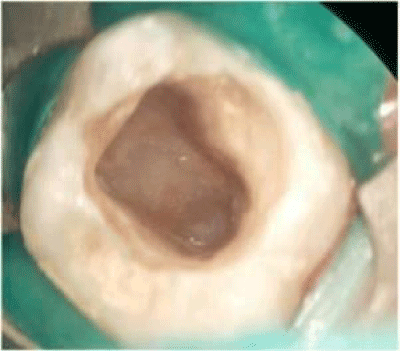
The endodontic treatment of tooth #26 was performed first. The access cavity was prepared after rubber dam isolation. A large pulp chamber filled entirely by the pulp tissue was encountered. Inspection of access cavity and exploration of canals was performed under dental operating microscope (Figure 3). Magnifying loupes (Carl Zeiss, India) were used throughout the procedure to facilitate visualization. 5.2% sodium hypochlorite was used as irrigating solution and was activated with the help of ultrasonics. The furcation area was situated in the apical third region and four canal orifices were located at the furcation area; mesiobuccal (MB1), second mesiobuccal (MB2), distobuccal and palatal.
Figure 3: Access cavity preparation showing apical position of pulpal floor observed under DOM (8x) of #26.
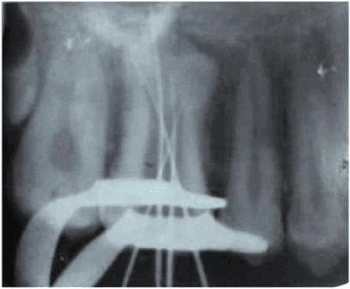
Working length determination was performed using electronic apex locator Root ZX (J Morita) and was confirmed with a radiograph (Figure 4). After working length determination the instrumentation of the canals was done using hybrid technique. Due to complexity of inner root canal anatomy, a modified obturation technique was employed; consisting of combined lateral condensation of the gutta percha in the apical part with vertical compaction of the remaining pulp chamber. AH-plus (Dentsply Detrey, USA) was used as a root canal sealer. The final radiograph was advised to evaluate complete obturation of root canal system. Similar procedure was followed in tooth #16. (Figure 5a,5b).
CASE 2
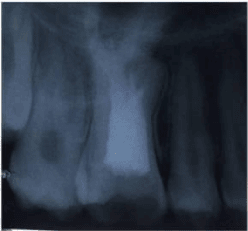
A 20-year-old healthy male patient reported to Department of Conservative dentistry and Endodontics with pain in lower left posterior region. Intraoral examination revealed the deep proximal caries in tooth #37 which was sensitive to percussion and palpation. Intraoral periapical radiograph of tooth #37showed huge pulp chamber extending beyond the CEJ reaching the furcation in the apical third region (Figure 6). Two short roots were seen at the furcation area in the apical third indicating hypertaurodontism. The contralateral tooth showed no such abberation. The diagnosis of irrevesible pulpitis with apical periodontitis and unilateral hypertaurodontism was made. Similar treatment procedure was carried out as in case 1 and final radiograph was taken that confirmed well obturated root canals in tooth #37 (Figure 7).
DISCUSSION
Taurodontism appears most frequently as an isolated anomaly; but it has been found to be associated with several syndromes and anomalies including Klinefelter’s, Down’s, tricho-dento-osseous syndrome, Mohr’s syndrome, Apert syndrome and others [5]. The greatest number of taurodonts observed in patients without any syndromes has been reported to be 10 [17]. The present case report shows 2 taurodonts in a patient with no known specific syndromes. Similar cases of bilateral taurodontism involving first maxillary molars have been reported in the literature [18,19]. Taurodontism can be associated with Oligodontia which is an uncommon genetic condition representing the congenital missing of six teeth or more in primary or permanent dentitions [20]. Taurodontism is a dental anomaly characterized by a distinct morphology which has given it a name as “bull teeth” [21,22]. In the presented cases, both patients had no systemic disease or any syndrome [23,24]. Most reports in the literature revealed that permanent teeth are more frequently affected than deciduous teeth [14]. Mandibular molars are found to be affected more often than maxillary molars [25]. Taurodontism of the premolars was reported by Tiku et al. [26]. The teeth that were diagnosed as taurodont in both the cases were of hyper taurodontism type.
This case report used the biometric method suggested by Shifman and Chanannel [16]. The classification of taurodontism suggested by Shaw [13] can be obtained by this biometric method. According to this index system [16] hypotaurodontism is diagnosed when TI is 20-30, mesotaurodontism when TI is 30-40, and hypertaurodontism when TI is 40-75. In present case reports, 3 teeth including right maxillary first molar, left maxillary first molar and lower left second molar showed hypertaurodontism.
Usually a taurodont shows wide variation in the size and shape of the pulp chamber with varying degrees of obliteration and canal configuration. Diagnosis of taurodontism is relatively easy with CBCT giving information regarding the exact location of bifurcation or trifurcation. However, endodontic management of such teeth is much more challenging than the routine cases. Problems may be faced in visualization of canal orifices as the pulpal floor is too far apically giving false feeling of perforation and hence making the negotiation of canals challenging. In such cases, debridement of pulp tissue from the large pulp chamber is more time consuming than routine cases. Hence a combination of various hand and rotary instruments with recommended use of ultrasonic irrigation using 5.2% sodium hypochlorite is mandatory to ensure complete debridement. The contributing factors for the successful endodontic treatment in such cases include careful exploration of the grooves between all the orifices particularly with magnification, ultrasonic irrigation and modified obturation techniques [27].
CONCLUSION
Although Taurodontism is a dental rarity and a challenge to the dentist, thorough knowledge of dental anatomy, radiographic examination and its association with other syndromes of this dental rarity should be well-understood. The combined use of modern diagnostic aids and treatment facilities as well as the clinicians’ skill and acumen are instrumental for successful endodontic outcome of taurodontism.
REFERENCES
- Neville BW, Damm DD, Allen CM, Bouquot JE. Oral & Maxillofacial Pathology. 5th edn. Philadelphia: WB Saunders, 2002.
- Jafarzadeh H, Azarpazhooh A, Mayhall JT. Taurodontism: a review of the condition and Endodontic treatment challenges. Int Endod J. 2008; 41: 375-388. Ref.: https://goo.gl/0gDJN4
- Durr DP, Campos CA, Ayers CS. Clinical significance of taurodontism. J Am Dent Assoc. 1980; 100: 378-381. Ref.: https://goo.gl/OGlZtw
- Llamas R, Jimenez-Planas A. Taurodontism in premolar. Oral Surg Oral Med Oral Pathol.1993; 75: 501-505. Ref.: https://goo.gl/qUP2AO
- Jaspers MT. Taurodontism in the Down syndrome. Oral Surg Oral Med Oral Pathol. 1981; 51: 632-636. Ref.: https://goo.gl/su5B80
- Schulman GS, Redford-Badwal D, Poole A, Mathieu G, Burleson J, et al. Taurodontism and learning disabilities. In patients with Klinefelter syndrome. Pediatr Dent. 2005; 27: 389-394. Ref.: https://goo.gl/6cPfNd
- Gros CI, Clauss F, Obry F, Manière MC, Schmittbuhl M, et al. Quantification of taurodontism: interests in the early Diagnosis of hypohidrotic ectodermal dysplasia. Oral Dis. 2010; 16: 292-298. Ref.: https://goo.gl/F6FVzh
- Tomona N, Smith AC, Guadagnini JP, Hart TC. Craniofacial and dental phenotype of Smith-Magenis syndrome. Am J Med Genet A. 2006; 140: 2556-2561. Ref.: https://goo.gl/GrO7ae
- Hazza’a AM, Al-Jamal G. Radiographic features of the jaws and teeth in thalassaemia major. Dentomaxillofac Radiol. 2006; 35: 283-288. Ref.: https://goo.gl/twPlw1
- Nguyen T, Phillips C, Frazier-Bower S, Wright T. Craniofacial variations in the tricho-dento-osseous syndrome. Clin Genet. 2013; 83: 375-379. Ref.: https://goo.gl/P8Ta4r
- Al jamal GA, Hazza’a AM, Rawashdeh MA. Prevalence of dental anomalies in a population of cleft lip and palate patients. Cleft Palate Craniofac J. 2010; 47: 413-420. Ref.: https://goo.gl/orxMMe
- Nawa H, Oberoi S, Vargervik K. Taurodontism and Van der Woude syndrome. Is there an association? Angle Orthod. 2008; 78: 832-837. Ref.: https://goo.gl/yGJEHd
- Shaw JC. Taurdont teeth in South African races. J Anat. 1928; 62: 476-498. Ref.: https://goo.gl/bkCUO3
- Goaz PW, White SC. Oral mRadiology (Principle and interpretation), 3rd edn St. Louis, Missouri: CV. Mosby Year Book Inc. 1994.
- Kosinski RW, Chaiyawat Y, Rosenberg L. Localized deficient root development associated with Taurodontism: case report. Pediatr Dent. 1999; 21: 213-215. Ref.: https://goo.gl/lYjK5Z
- Shifman A, Chanannel I. Prevalence of taurodontism found in radiographic dental Examination of 1,200 young adult Israeli patients. Community Dent Oral Epidemiol. 1978; 6: 200-203. Ref.: https://goo.gl/RlxFPK
- Radwan A, Kim SG. Treatment of a Hypertaurodontic Maxillary Second Molar in a Patient with 10 Taurodonts: A Case Report. J Endod. 2014; 40: 140-144. Ref.: https://goo.gl/DK8yd2
- Kavita Verma, Kapil Loomba, Rhythm Bains. Endodontic Management of a Hypertaurodont Maxillary First Molar Asian Journal of Oral Health & Allied Sciences 2012; 101-103.
- Simsek N, Keles A, Ocak MS. Endodontic treatment of hypertaurodontism with multiple bilateral Taurodontism. J Conserv Dent. 2013; 16: 477-479. Ref.: https://goo.gl/zjtPPx
- Santosh R Patil, Aileni Kaladhar Reddy J. Dental Research and Review 2015; 34-36.
- Joseph M. Endodontic treatment in three taurodontic teeth associated with 48, XXXY Klinefeltor syndrome: A review and case report. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2008; 105: 670-677. Ref.: https://goo.gl/9jlwrF
- Dineshshankar J, Sivakumar M, Balasubramanium AM, Kesavan G, Karthikeyan M, et al. Taurodontism. J Pharm Bioallied Sci. 2014; 6: 13-15. Ref.: https://goo.gl/92X5Cq
- Genc A, Namdar F, Goker K, Atasu M. Taurodontism in association with super numerary teeth. J Clin Pediatr Dent. 1999; 23: 151-154. Ref.: https://goo.gl/3Pv47u
- Gedik R, Cimen M. Multiple Taurodontism: Report of a case. ASDC J Dent Child. 2000; 67: 216-217. Ref.: https://goo.gl/nNQjSe
- MacDonald-Jankowski DS, Li TT. Taurodontism in a young adult chinese population. DentoMaxillofac Radiol. 1993; 22: 140-144. Ref.: https://goo.gl/uW4oRv
- Tiku A, Damle SG, Nadkarni UM, Kalaskar RR. Hypertaurodontism in molars and premolars: Management of two rare cases. J Indian Soc Pedod Prev Dent. 2003; 21: 131-134. Ref.: https://goo.gl/pFIYKA
- Varrela J, Alvesalo L, Mayhall J. Taurodontism in 45, X females. J Dent Res. 1990; 69: 494-495. Ref.: https://goo.gl/uIs3CK