More Information
Submitted: December 24, 2021 | Approved: March 23, 2022 | Published: March 25, 2022
How to cite this article: Asha B, Rudrakshi C, Prabhuji MLV, Pireethi P. To estimate the levels of gingival crevicular fluid YKL-40 in patients with chronic periodontitis and rheumatoid arthritis with chronic periodontitis - a clinico-biochemical study. J Clin Adv Dent. 2022; 6: 010-016.
DOI: 10.29328/journal.jcad.1001026
Copyright License: © 2022 Asha B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Chronic periodontitis; Gingival crevicular fluid; Rheumatoid arthritis; YKL-40
To estimate the levels of gingival crevicular fluid YKL-40 in patients with chronic periodontitis and rheumatoid arthritis with chronic periodontitis - a clinico-biochemical study
Asha B, Rudrakshi C*, MLV Prabhuji and Pireethi P
Department of Periodontics, Krishnadevaraya College of Dental Sciences, Bangalore, Karnataka, India
*Address for Correspondence: Dr. Rudrakshi C, Reader, Department of Periodontics, Krishnadevaraya College of Dental Sciences and Hospital, Sir MVIT Campus, New Airport Road, Bengaluru-562157, Karnataka, India, Email: [email protected]
Background and objectives: YKL-40, a C-reactive protein belongs to the positive acute-phase protein. It is also known as Human chitinase-3-like protein 1(HCI3L1) and is closely related to both acute and chronic inflammation. The present study aimed to detect and estimate the levels of YKL-40 in gingival crevicular fluid (GCF) in patients with healthy periodontium, chronic periodontitis, and rheumatoid arthritis with chronic periodontitis.
Materials and methods: Forty-five patients in the age range of 25-55 years were included in the study. Patients were divided into three groups: Group I-15 Periodontal healthy patients, Group II-15 Chronic Periodontitis patients, and Group III-15 Rheumatoid arthritis with chronic periodontitis patients. Clinical parameters recorded were Plaque index, Gingival index, Gingival bleeding index, probing depth, and Relative attachment level. GCF samples were analyzed using ELISA. p - value < 0.05 was considered statistically significant.
Results: The highest mean YKL-40 concentration in GCF was observed in rheumatoid arthritis with Chronic periodontitis. The mean concentration of YKL-40 in GCF showed a three to four folds increase in its levels when compared to healthy controls (p < 0.001). Contrary, GCF YKL-40 levels between Group II and Group III were not significant.
Conclusion: With the increase in severity of periodontal destruction from healthy periodontium to chronic periodontitis, there was a substantial increase in the concentration of YKL-40 in GCF. Correlation of GCF YKL-40 with clinical parameters demonstrated increased severity of the diseases increased its levels.
The onset, progression, and severity of periodontal diseases are related to the interaction between periodontal micro-organism and host immune response [1]. It has been noted that periodontal pathogens like Porphyromonas gingivalis are able to invade gingival tissue [2] and are able to gain access to the systemic circulation [3]. This periodontal systemic disease interrelationship is believed to be mediated through systemic inflammatory reactants such as acute-phase proteins and immune effectors [4,5]. Recent evidences [6-9] suggest that periodontal infection may significantly enhance the risk for various systemic diseases.
The similarities between rheumatoid arthritis and chronic periodontitis exist both at the cellular and molecular level [10]. However, study [11] have reported an increased prevalence of rheumatoid arthritis in a patient with periodontal diseases. Treatment of periodontal disease has demonstrated a significant reduction in erythrocyte sedimentation rate (ESR) which in turn has shown improvement of clinical indices on rheumatoid arthritis activity [12]. Recently isolated molecule in human serum and synovial fluids is a 40- kDa protein, YKL- 40 (human cartilage glycoprotein-39) [HC-gp39]. It is an acute-phase protein, a novel potential inflammatory marker for both acute and chronic inflammation [13].
YKL-40 is also known as Human Chitinase-3-like Protein 1(CHI3L1). The amino acid sequence of YKL -40 is related to the chitinase protein family, but it has no chitinase activity [14]. Previous study [15] showed that plasma concentration of YKL-40 increases reversibly > 25% after an inflammatory stimulus. Serum or plasma levels of YKL-40 are higher in patients with several systemic diseases characterized by inflammation, such as rheumatoid arthritis [8,9], osteoarthritis [16], coronary arteries diseases [15] myocardial infarction (MI) [17] etc. Serum YKL-40 level in patients with clinically active rheumatoid arthritis was found to be higher than that of clinically inactive patients and was decreased by steroid treatment [18]. Studies [19,20]. linking the presence of YKL-40 in inflammatory periodontal diseases has positively co-related with other inflammatory cytokines (IL-6, TNF-α, etc.).
Hence, we speculated the presence of YKL-40 in both chronic periodontitis and rheumatoid arthritis. The purpose of this study was to detect and estimate the levels of YKL-40 in gingival crevicular fluid (GCF) of a patient with healthy gingiva, chronic periodontitis, and rheumatoid arthritis with chronic periodontitis and to correlate with clinical parameters of periodontal disease.
Patients were recruited from Government general hospital, Yelahanka, Bangalore 560064. From the outpatient section, Department of Periodontology, KCDS, Patients with healthy periodontium, chronic periodontitis, and rheumatoid arthritis having chronic periodontitis were included in the study. A total of 45 patients were divided into the following groups: Group I (Healthy/control) 15 subjects (2 males & 13 females), Group II (Chronic periodontitis) 15 subjects (6 males & 9 females), and Group III (Rheumatoid arthritis with chronic periodontitis) 15 subjects (3 males & 12 females) aged 25-55 years. The subjects have informed of the nature, potential risks, and benefits of their participation in the study, and an informed signed consent was obtained.
The study approval was obtained from the Institutional Review Board and Ethical Committee (Ref. No. KCDS/165 /2018-19) on 22/10/2018 of Krishnadevaraya College of Dental Sciences and Hospital, affiliated to the Rajiv Gandhi University of Health Sciences, Bangalore, Karnataka, India. The clinical trial registry was done with registration number: NCT03995615.
Patients satisfying the following inclusion and exclusion criteria were included. Inclusion criteria were patients with generalized initial to moderate chronic periodontitis, patients with active rheumatoid arthritis diseases considered according to 1987 revised classification criteria of the American rheumatism association, as well as the 2010 Rheumatoid factor classification criteria of the American college of rheumatology and European League Against Rheumatism having seropositive for Rheumatoid factor (RA) with a DAS scoring between ≥ 3.2 to ≤ 5.1, a patient who had not received any periodontal treatment in last six months, and a patient who are co-operative and were able to attend follow-up. Exclusion criteria were any systemic diseases such as diabetic Mellitus and thyroid diseases, former and current smokers, pregnant and lactating females, and use of antibiotics or Diseases Modifying Anti-Rheumatic Drugs (DMARD) that affects the periodontal status in the last six months.
Criteria for grouping
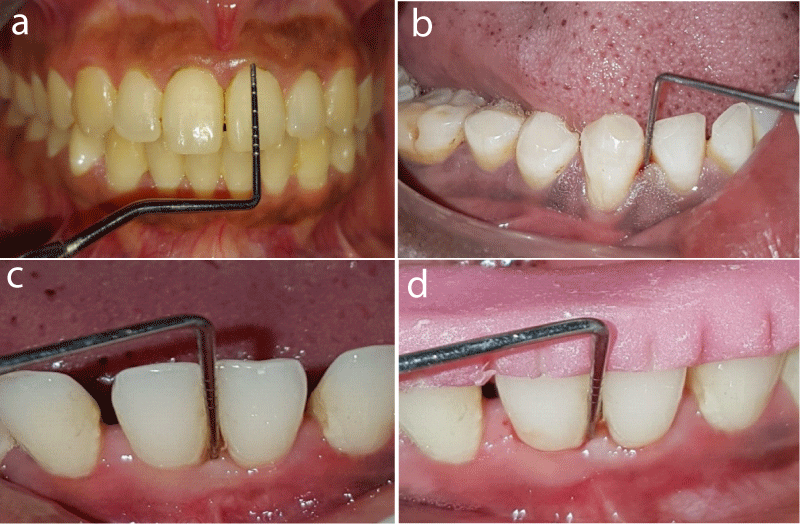
Group I (Control): 15 healthy subjects having probing depth < 3 mm and ≤ 10% sites with bleeding on probing (Figure 1a).
Group II: 15 healthy subjects with chronic periodontitis patients having probing depth ≥ 4 mm and relative attachment level ≥ 3 mm, ≥ 25% of sites with gingival bleeding (Figure 1b).
Group III: 15 Rheumatoid arthritis patients with DAS between ≥ 3.2 to ≤ 5.1 having chronic periodontitis with probing depth ≥ 5 mm, relative attachment loss of ≥ 8 mm and ≥ 10% sites with bleeding on probing (Figure 1c).
Clinical parameters recorded: Plaque Index (PI), Gingival Index (GI), Gingival Bleeding Index (GBI), Periodontal Pocket Depth (PPD), and Relative Attachment Levels (RAL) (Figure 1d) using graduated Williams’s periodontal probe.
Figure 1: a) Group I: Healthy periodontium ; b) Group II: Chronic periodontitis with probing depth of > 4 mm; c) Group III: Rheumatoid arthritis with chronic periodontitis with probing depth of > 4 mm; d) Measurement of Relative attachment level.
GCF collection: GCF samples were collected using absorbable paper strips Periocol, ORAFLOW®, USA paper strips by extra sulcular method. Periocol strip was placed into the sulci/pocket gently until mild resistance was sensed. It was left in place for the 30s. Samples contaminated by saliva or blood were discarded. A total of 45 GCF samples were collected for analysis. Volumetric analysis was done using Periotron 8000 and readings were recorded. Samples were placed in an Eppendorf tube containing 200 μL of PBS. To elute the GCF from paper strips, the tubes were centrifuged for 5 minutes at 3000 rpm to remove plaque and cellular elements. The strips were removed and the samples were stored at -80 oC until further use.
Estimation of YKL-40 with ELISA
YKL-40 levels in GCF were determined by using an ELISA kit. Immunoassay was done according to manufacturer’s instructions (KINESIS Dx)® The ELISA kit uses sandwich enzyme-linked immunosorbent assay to assay the level of Human Chitinase-3-like Protein 1(CHI3L1) in samples. Chitinase-3-like Protein 1(CHI3L1) is added to wells pre-coated with monoclonal Chitinase-3-like Protein 1(CHI3L1) antibody. After incubation, added secondary antibodies labeled with biotin followed by Streptavidin-HRP to form an immune complex. Unbound immune complex is removed by washing step. Then the addition of Chromogenic Solution A and B develops blue color and a stop solution is added to stop the reaction. Samples analyses were repeated to confirm. The concentration of CHI3L1 was directly proportional to the color developed. The absorbance of the reacting solution in wells was determined at 450 nm. The concentrations of YKL-40 are expressed as picograms per microliter.
Statistical analysis
The mean value, standard deviation (SD), minimum and maximum age distribution of the study population were calculated using Kruskal Walli’s test and gender distribution between three groups using the Chi-Square test. Independent Student t - test was used to compare the mean RAL levels between Group II & III. For the non-parametric test, the Kruskal Wallis test followed by Mann Whitney post hoc analysis was used to compare the mean YKL-40 levels [in pg/ml] between three study groups. The level of significance was set at p < 0.05. Spearman’s Correlation test was performed to assess the relationship between YKL-40 levels and other study parameters in each study group.
Comparison of various clinical parameters between groups
The mean PI, GI, GBI, and PD scores between Group I versus Group II and between Group I versus Group III were found statistically significant (p < 0.001), between Group II versus Group III, showed no statistically significant (Table 1).
| Table 1: Intergroup comparison between Group I, Group II, and Group III. | ||||
| Parameters | Sig. Diff | N | Mean | p - valueb |
| Plaque Index | Group I vs. Group II | 15 | 0.49 vs. 1.58 | < 0.001* |
| Group I vs. Group III | 15 | 0.49 vs. 1.37 | < 0.001* | |
| Group II vs. Group III | 15 | 1.58 vs. 1.37 | 0.45 | |
| Gingival Index | Group I vs. Group II | 15 | 0.59 vs. 1.69 | 0.008* |
| Group I vs. Group III | 15 | 0.59 vs. 1.73 | < 0.001* | |
| Group II vs. Group III | 15 | 1.69 vs. 1.73 | 0.15 | |
| Gingival bleeding Index |
Group I vs. Group II | 15 | 1.52 vs. 5.97 | < 0.001* |
| Group I vs. Group III | 15 | 1.52 vs. 6.81 | < 0.001* | |
| Group II vs. Group III | 15 | 5.97 vs. 6.81 | 0.57 | |
| Probing depth | Group I vs. Group II | 15 | 1.47 vs. 6.13 | < 0.001* |
| Group I vs. Group III | 15 | 1.47 vs. 6.67 | < 0.001* | |
| Group II vs. Group III | 15 | 6.13 vs. 6.67 | 0.37 | |
| *p ≤ 0.001 - Statistically significant; Note: b. p - value derived by Tukey's post hoc test. | ||||
Comparison of RAL between Group II and Group III: The mean RAL score showed no difference between GroupII and GroupIII, which was statistically not significant (p = 0.26 and p = 0.55) (Table 2).
| Table 2: Comparison of mean Relative attachment levels between Group II & Group III. | ||||||
| Parameter | Group | N | Mean | SD | Mean Diff | p - Value |
| Relative attachment level | Group II | 15 | 8.87 | 0.83 | -0.20 | 0.55 |
| Group III | 15 | 9.07 | 0.96 | |||
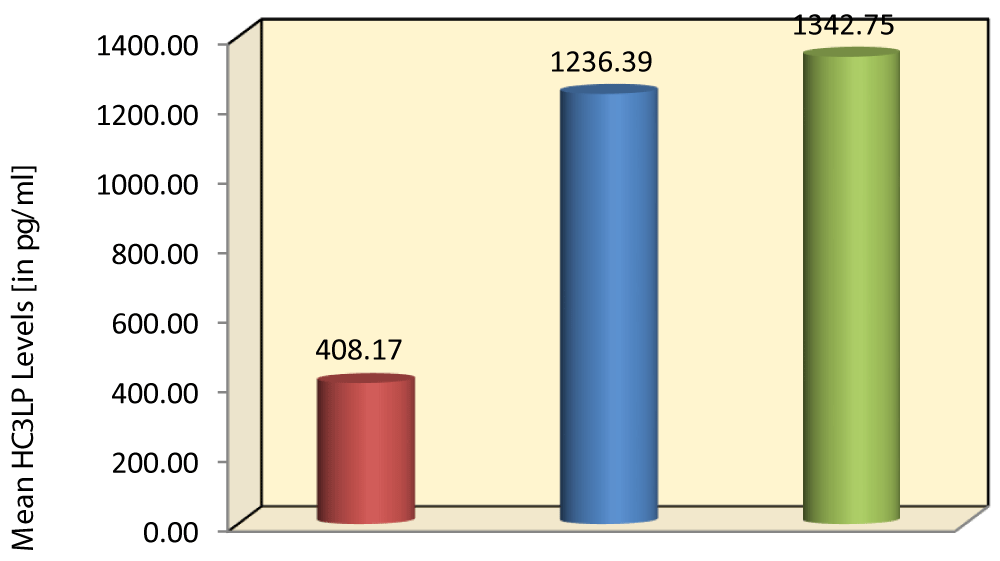
Comparison of YKL-40 level among all three groups: The mean YKL-40 concentration of GCF in Group I, Group II, and Group III were 408.17 pg/ml, 1236.39 pg/ml, and 1342.75 pg/ml. (Graph 1). The mean YKL-40 levels in GCF between Group I versus Group II (408.17 vs. 1236.39) and between Group I versus Group III (408.17 vs. 1342.75) were found to be statistically significant (p < 0.001), between Group II versus Group III (1236.39 vs. 1342.75) showed no statistical significance (p = 0.22) (Table 3).
Graph 1: Comparison of mean GCF YKL-40 levels (pg/ml) among the study group.
| Table 3: Intergroup comparison of GCF YKL-40 between three groups. Comparison of mean GCF YKL-40 (pg/ml) b/w 3 study groups using Kruskal Wallis Test followed by Mann Whitney post hoc Analysis | |||||||||
| Parameters | Groups | N | Mean | SD | Min | Max | p - valuea | Sig. Diff | p - valueb |
| GCF YKL-40 (pg/ml) | Group I | 15 | 408.17 | 139.19 | 157.6 | 639.7 | < 0.001* | Group I vs. Group II | < 0.001* |
| Group II | 15 | 1236.39 | 97.90 | 983.6 | 1376.5 | Group I vs. Group III | < 0.001* | ||
| Group III | 15 | 1342.75 | 269.93 | 934.4 | 1745.8 | Group II vs. Group III | 0.22 | ||
| *p ≤ 0.001 Statistically significant; Note: b. p - value derived by Mann Whitney post hoc test. | |||||||||
Correlation between YKL-40 level and clinical parameters: Correlation of GCF YKL-40 with clinical parameters demonstrated increased severity of the diseases increased its levels. A moderate to strong correlation was shown in all the clinical parameters between Group II and Group III patients. Whereas Group I showed a negative correlation with the clinical parameters (PI, GI, GBI, and PD) (Table 4).
| Table 4: Correlation of GCF YKL- 40 and clinical parameters between three groups. | |||||||
| Group | Variable | Values | PI | GI | BOP | PD | RAL |
| Group I | GCF YKL-40 | rho | -0.01 | -0.49 | 0.00 | -0.22 | NA |
| p - value | 0.98 | 0.07 | 0.99 | 0.44 | NA | ||
| Group II | GCF YKL-40 | rho | 0.64 | 0.61 | 0.64 | 0.69 | 0.63 |
| p - value | 0.01* | 0.02* | 0.01* | 0.005* | 0.01* | ||
| Group III | GCF YKL-40 | rho | 0.62 | 0.60 | 0.63 | 0.67 | 0.56 |
| p - value | 0.01* | 0.02* | 0.01* | 0.007* | 0.03* | ||
| * p ≤ 0.001 - Statistically significant; Correlation coefficient range 0.0 - No Correlation 0.01 - 0.20 - Very Weak Correlation 0.21 - 0.40 - Weak Correlation 0.41 - 0.60 - Moderate Correlation 0.61 - 0.80 - Strong Correlation 0.81 - 1.00 - Very Strong Correlation |
|||||||
Rheumatoid arthritis (RA) leads to systemic inflammation at a chronic level, affecting adversely the cartilage and bones pertaining to small joints of the limbs. This may cause contrasting degrees of deformity and functional disability [22]. PD was found affiliating with RA, despite the fact that the etiologies of the two conditions are different [23] the reason may be attributed to the similarity of the underlying pathological processes, such that individuals in danger of acquiring one condition are also at risk for the other [10]. Porphyromonas gingivalis (Pg) was found significantly present in periodontitis, and it is also correlated with the occurrence of RA [23]. Antibodies associated with RA have also been detected in periodontitis patients not suffering from RA [22]. Inflamed periodontal tissues also show increased levels of cyclic citrullinated proteins (CCPs), along with the presence of anti-citrullinated protein antibody (ACPAs) in GCF, saliva, and serum of patients of RA [22,24]. As well as CP [24]. Studies investigating the role of post-translation modification of proteins (ACPA) in the association between RA and PD have shown an association with PD severity and influenced by periodontal treatment with RA [26-28].
YKL-40 is a C-reactive protein that belongs to the positive Acute Phase Proteins (APP) variety [29]. Growing clinical evidence shows that increased secretion of YKL-40 is related to the pathogenesis of a variety of inflammatory diseases. Studies investigating the relationship between YKL-40 and periodontal diseases have indicated an association between YKL-40 levels and periodontal diseases in gingival crevicular fluid (GCF) [19,30-32] and serum [33]. Therefore, YKL-40 is not a disease-specific molecule, seems to be a potential mediator in inflammatory diseases [13].The expression of YKL-40 an acute phase protein in both rheumatoid arthritis (Volck’s 2001 and Peltom 2001) [16,34] and periodontitis (Keles 2014 and Kedo 2015) [19,31]. was seen.
In the present study, the mean PI, GI, GBI, and PD scores for Group II and Group III patients were significantly higher than in the control group (Group I). Furthermore, on the intergroup comparison, the difference in mean PI, GI, and GBI scores was statistically highly significant (p ≤ 0.001). Similar observations were made by Keles, et al. [19], Kido, et al. [31], Zhao, et al. [35] and Rodriguez Lozano, et al. [36], reported higher PI, GI, and GBI scores in rheumatoid arthritis with chronic periodontitis (RAPD) patients than in a healthy group. This finding validates the positive role played by the local factors in the etiopathogenesis of gingival and periodontal disease. In our study, occlusal stents were prepared for CP and RAPD patients and RAL was calculated. Comparison between Group II and Group IIII did not show any statistically significant difference, where the p < 0.55. These results were contrary to Keles, et al. [19,32], where they compared CAL between healthy/gingivitis and chronic periodontitis (p < 0.05). Zhao, et al. [35] demonstrated the highly significant (p < 0.001) difference between healthy and rheumatoid arthritis patients. In the study done by Damodar, et al. [30], the intra-and intergroup comparison showed a statistically significant difference (p < 0.001) in CAL parameters in patients with and without diabetes mellitus (DM), six weeks post-intervention (Scaling and Root planning).
In our study, the GCF concentration of YKL-40 was found highest in Group III patients followed by Group II, and least in Group I. On intergroup comparison, the difference in the mean GCF concentration of YKL-40 was statistically highly significant (p ≤ 0.001). According to Keles, et al. [19], the level of GCF YKL-40 in CP patients is greater than in healthy controls. According to Kido et al. [31], the level of GCF YKL-40 in CP patients with and without diabetes is greater than in healthy controls. Keles, et al. [32] and Damodar, et al. [30] reported that baseline mean GCF YKL-40 level reduced at 6 weeks post periodontal therapy.
The present study clearly shows that the total amount of GCF YKL-40 was higher in periodontal tissue breakdown. YKL-40 is considered to be associated with the severity of periodontal diseases. GCF YKL-40 levels between Group II and Group III were not significant. The hypothetical explanation for this is due to elevated levels of YKL-40 detected in GCF of chronic periodontitis patients and rheumatoid arthritis with chronic periodontitis patients might be due to YKL-40 produced locally by inflammatory cells in the periodontium. This substantiates similarity in the pathogenesis of rheumatoid arthritis and periodontitis. The mean concentration of YKL-40 in GCF showed a three to four folds increase in its levels when compared to healthy controls (p < 0.001). Correlation of GCF YKL-40 with clinical parameters demonstrates a moderate to strong correlation was shown in all the clinical parameters between Group II and Group III patients. Whereas Group I showed a negative correlation with the clinical parameters (PI, GI, GBI, and PD). The study had some limitations: 1. The small size of the study was with the p - value < 0.05. 2. Gingivitis group was not included. 3. Periodontal intervention was not considered for CP and RA with CP patients. Further studies, with larger sample size and estimating changes of YKL 40 levels with intervention are required.
The present study indicates that GCF YKL-40 was minimum for Group I patients and maximum for Group III patients. YKL-40 levels were intermediate in Group II patients. With the increase in severity of periodontal destruction from healthy periodontium to chronic periodontitis, there was a substantial increase in the concentration of YKL-40 in GCF. YKL-40levels in GCF were positively correlated with all clinical parameters only in Group II and Group III patients. The measurement of YKL-40 in GCF samples may be used as a novel marker for periodontal disease activity.
- Schenkin HA. Informational paper. The pathogenesis of periodontal diseases. J Periodontol. 1999; 70: 457- 470. PubMed: https: //pubmed.ncbi.nlm.nih.gov/10328661/
- Sandros J, Papapanau PN, Nan mark U, Dahlen G. Porphyromonas gingivalis invades human pocket epithelium in vitro. J Periodontal Res. 1994; 29: 62-69. PubMed: https: //pubmed.ncbi.nlm.nih.gov/8113953/
- Harsazthy VI, Ambo JJ, Trevisan M, Zeid M, Genco. Identification of periodontal pathogen in atheromatous plaques. J Periodontal. 2000; 71: 1554-1560. PubMed: https: //pubmed.ncbi.nlm.nih.gov/11063387/
- Sandros J. Karlsson C, Lappin DF, Madianos PN, Kinane DF, et al. Cytokines response of oral epithelia cells to P. gingivalis infection. J Dent Res. 2000; 79: 1808-1814. PubMed: https: //pubmed.ncbi.nlm.nih.gov/11077999/
- Dye BA, Chaudhary K, Shea S, Papapanou PN. Serum antibodies to periodontal pathogen and marker of systemic inflammation. J Clin Periodontal. 2005; 32: 1189-1199. PubMed: https: //pubmed.ncbi.nlm.nih.gov/16268994/
- Bartold PM, Marshall RI, Haynes DR. Periodontitis and rheumatoid arthritis: a review. J Periodontal. 2005; 76: 2066-2074. PubMed: https: //pubmed.ncbi.nlm.nih.gov/16277578/
- Marotte H, Farge P, Gaudin P, Miossec P. The association between periodontal diseases and joint destruction in rheumatoid arthritis extends the link between the HLA-DR shared epitope and severity of bone destruction. Ann Rheum Dis. 2006; 65: 905-909. PubMed: https: //pubmed.ncbi.nlm.nih.gov/16284099/
- Lenartova M, Tesinska B, Janatova T, Hrebicek O, Mysak J, et al. The Oral Microbiome in Periodontal Health. Front Cell Infect Microbiol. 2021; 11: 629723. PubMed: https: //pubmed.ncbi.nlm.nih.gov/33828997/
- Koziel J, Potempa J. Pros and cons of causative association between periodontitis and rheumatoid arthritis. Periodontol. 2000. PubMed: https: //pubmed.ncbi.nlm.nih.gov/35262966/
- Mercado FB, Marshall RI, Klestov AC, Garbarsch C, Relationship between rheumatoid arthritis and periodontitis. J Periodontal. 2001; 72: 779-787. PubMed: https: //pubmed.ncbi.nlm.nih.gov/11453241/
- Persson GR. Rheumatoid arthritis and periodontitis inflammatory and infectious connections. Review of the literature. J Oral Microbiol. 2012; 4: 11829. PubMed: https: //pubmed.ncbi.nlm.nih.gov/22347541/
- Riberio J, Leao A. Novae AB. Periodontal infection as a possible severity factor for RA. J Clin Periodontol. 2005; 32: 412-416. PubMed: https: //pubmed.ncbi.nlm.nih.gov/15811060/
- Johnsen JS, Johnsen HS, Price PA a New biochemical marker for joint injury. Analysis of YKL-40 in serum and synovial fluid. Br J Rheumatol. 1993; 32: 949–955. PubMed: https: //pubmed.ncbi.nlm.nih.gov/8220933/
- Hakala BE, White C, Recklies AD. Human cartilage gp- 39, a major secretory product of articular chondrocytes and synovial cells, is a mammalian member of a chitinase protein family. J Biol Chem 1993; 268: 25803–25810. PubMed: https: //pubmed.ncbi.nlm.nih.gov/8245017/
- Roslind A, Johansen JS. YKL-40: A novel marker shared by chronic inflammation and oncogenic transformation. Methods Mol Biol. 2009; 511: 159-184. PubMed: https: //pubmed.ncbi.nlm.nih.gov/19347297/
- Peltomaa R, Paimela L, Harvey S, Helve T, Leirisalo- Repo M. Increased level of YKL-40 in sera from patients with early rheumatoid arthritis: A new marker for disease activity. Rheumatol Int. 2001; 20: 192-196. PubMed: https: //pubmed.ncbi.nlm.nih.gov/11518039/
- Rathcke CN, Vestergaard H. YKL-40 -An emerging biomarker in cardiovascular disease and diabetes. Cardiovasc Diabetol. 2009; 8: 61.
- Johansen JS, Stoltenberg M, Hansen M. Serum YKL-40 concentrations in patients with rheumatoid arthritis: relation to disease activity. Rheumatology. 1999; 38: 618–626. PubMed: https: //pubmed.ncbi.nlm.nih.gov/10461474/
- Keles ZP, Keles GC, Avci B, Cetinkaya BO, Emingil G. Analysis of YKL‐40 acute‐phase protein and interleukin‐6 levels in periodontal disease. J Periodontol. 2014; 85: 1240-1246. PubMed: https: //pubmed.ncbi.nlm.nih.gov/24635545/
- Ozmeric N. Advances in periodontal disease markers. Clini Chimi Acta. 2004; 343: 1-16. PubMed: https: //pubmed.ncbi.nlm.nih.gov/15115674/
- Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol. 2015; 15: 30-44. PubMed: https: //pubmed.ncbi.nlm.nih.gov/25534621/
- Indurkar MS, Bhailume PS, Raut AS. Is periodontitis and rheumatoid arthritis inter‑related. J Interdiscip Med Dent Sci. 2018; 6: 231.
- Jung ES, Choi YY, Lee KH. Relationship between rheumatoid arthritis and periodontal disease in Korean adults: Data from the Sixth Korea National Health and Nutrition Examination Survey, 2013 to 2015. J Periodontol. 2019; 90: 350‑357. PubMed: https: //pubmed.ncbi.nlm.nih.gov/30380152/
- Rutter Locher Z, Fuggle N, Orlandi M, D’Aiuto F, Sofat N. Periodontal disease and autoimmunity: What we have learned from microbiome studies in rheumatology. In: Arjunan P, editor. Text Book of Periodontitis – A Useful Reference. 1st ed. London: Intech Open Publishers. 2017; 113-141.
- Harvey GP, Fitzsmmons TR, Dhamarpatni AA. Expression of peptidylarginine deiminase-2 and-4, citrullinated proteins anti citrullinated protein antibodies in human gingiva. J Periodontal Res. 2013; 48: 252-261. PubMed: https: //pubmed.ncbi.nlm.nih.gov/22978559/
- Mankia K, Cheng Z, Do N, Hunt L, Meade J, et al. An increased prevalence of periodontal disease and Porphyromonas gingivalis in anti-CCP positive individuals at-risk of rheumatoid arthritis: a target for prevention? JAMA Netw Open. In Press 2019.
- Bright R, Thiele GM, Manavis J, Mikuls TR, Payne JB, et al. Gingival tissue, an extra synovial source of malondialdehyde acetaldehyde adducts citrullinated and carbamylated proteins. J Periodontal Res. 2018; 53: 139-143. PubMed: https: //pubmed.ncbi.nlm.nih.gov/29044530/
- Kaneko C, Kobayashi T, Ito S, Sugita N, Murasawa A, et al. Circulating levels of carbamylated protein and neutrophil extracellular traps are associated with periodontitis severity in patients with rheumatoid arthritis: a pilot case-control study. PLoS ONE. 2018; 13: e0192365. PubMed: https: //pubmed.ncbi.nlm.nih.gov/29394286/
- Polepalle T, Moogala S, Boggarapu S, Pesala DS, Palagi FB. Acute phase proteins and their role in periodontitis: A Review. J Clin Diagn Res. 2015; 9: 01-05. PubMed: https: //pubmed.ncbi.nlm.nih.gov/26674303/
- Damodar S, Mehta DS. Effect of scaling and root planing on gingival crevicular fluid level of YKL-40 acute phase protein in chronic periodontitis patients with or without type 2 diabetes mellitus: A clinico-biochemical study. J Indian Soc Periodontol. 2018; 22: 40. PubMed: https: //pubmed.ncbi.nlm.nih.gov/29568171/
- Kido J, Bando Y, Bando M, Kajiura Y, Hiroshima Y, et al. YKL-40 level in gingival crevicular fluid from patients with periodontitis and type 2 diabetes. Oral Dis. 2015; 21: 667–673. PubMed: https: //pubmed.ncbi.nlm.nih.gov/25740558/
- Yucel ZPK, Keles GC, Avci B, Cetinkaya BO. Nonsurgical Periodontal Therapy Reduces Salivary and Gingival Crevicular Fluid YKL-40 and IL-6 Levels in Chronic Periodontitis. Oral Health Amp Prevent Dentis. 2020; 18: 4. PubMed: https: //pubmed.ncbi.nlm.nih.gov/32895666/
- Chavan V, Sabavath S, Babu CH, Boyapati L. Estimation of YKL-40 acute-phase protein in serum of patients with periodontal disease and healthy individuals: A clinical-biochemical study. Contemp Clin Dent. 2019; 10: 249. PubMed: https: //pubmed.ncbi.nlm.nih.gov/32308286/
- Johansen JS, Drivsholm L, Price PA, Christensen IJ. High serum YKL-40 level in patients with small cell lung cancer is related to early death. Lung Cancer. 2004; 46: 333-340. PubMed: https: //pubmed.ncbi.nlm.nih.gov/15541818/
- Zhao R, Gu C, Zhang Q, Zhou W, Feng G, et al. Periodontal disease in Chinese patients with rheumatoid arthritis: A case control study. Oral Dis. 2019; 25: 2003-2009. PubMed: https: //pubmed.ncbi.nlm.nih.gov/31411781/
- Rodriguez‐Lozano B, Gonzalez‐Febles J, Garnier‐Rodríguez JL, Dadlani S, Bustabad‐Reyes S, et al. Association between severity of periodontitis and clinical activity in rheumatoid arthritis patients: A case‐control study. Arthritis Res Ther. 2019; 21: 2. PubMed: https: //pubmed.ncbi.nlm.nih.gov/30658685/