More Information
Submitted: July 21, 2022 | Approved: August 04, 2022 | Published: August 05, 2022
How to cite this article: Park SY. Teledentistry and Digital Therapeutics (DTx) for dentistry. J Clin Adv Dent. 2022; 6: 028-030.
DOI: 10.29328/journal.jcad.1001029
Copyright License: © 2022 Park SY. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Teledentistry and Digital Therapeutics (DTx) for dentistry
Sang-Yoon Park*
Department of Oral and Maxillofacial Surgery, School of Dentistry, Seoul National University, Seoul, Korea
*Address for Correspondence: Sang-Yoon Park, Department of Oral and Maxillofacial Surgery, School of Dentistry and Dental Research Institute, Seoul National University, 101 Daehak-ro, Jongno-gu, Seoul 03080, Korea, Email: [email protected]
Due to the global pandemic spread of COVID-19, the medical field has experienced many changes [1]. One of the main changes is the attention to Telemedicine (Digital Medicine), which is a part of Digital Health. The combination of ‘Digital’ and ‘Dentistry’ can be awkward because dental treatment is often conducted face-to-face with clinical treatment, but it is planned to proceed with the inevitable flow of the times [2,3]. In addition, Digital therapeutics (DTx), a part of digital dentistry, is a narrower concept and has an evidence-based effect on diseases. This article contains opinions on the concept and current status of Teledentistry and the application of DTx [4].
In the case of the existing digital health, it has been introduced as a concept for personal health management and has received steady development and attention. However, the demand and development of digital medicine that is one step higher than this low-level medicine did not grow rapidly. However, the demand for telemedicine has increased due to the development of technologies such as artificial intelligence (AI), Internet of Things (IoT), Virtual reality (VR) and Augmented reality (AR) along with the spread of smartphones [5,6]. Currently, the development of telemedicine and digital medicine is progressing mainly in the United States and Europe [7]. In the case of dental treatment, because of the face-to-face treatment environment, the concept of digital medicine was slow to change in dentistry, and many dentists had difficulty adapting. However, amid the COVID-19 pandemic, the demand for digital medicine and digital dentistry has exploded. In addition, an environment for implementing many uses was prepared. In the case of digital therapeutics (DTx), it is a concept applied to digital medicine or digital dentistry of a slightly narrower concept. It is therapeutic that is involved in the diagnosis, management, and treatment of specific diseases. Characteristically, unlike the previous concepts, it must be proven to have an Evidence-based effect. Most of them are also software-based.
Digital health
Looking at the concept of digital health announced by the FDA in 2020, ‘The broad scope of digital health includes categories such as mobile health (mHealth), health information technology (IT), wearable devices, telehealth and telemedicine and personalized medicine. Is defined as Digital health. Digital health is a broad concept and it can be seen as the use of digital technology for the purpose of improving patient health [8,9].
Digital medicine
A broader definition of digital medicine is a field that is concerned with the use of technologies for measurement and intervention in the context of human health. As hardware and software using digital technology, it is aimed at individual treatment, recovery, disease prevention, and health promotion. In the case of digital medicine, it can be used independently or in combination with existing treatment techniques [8,10].
Digital therapeutics
The definition of digital therapeutics can be “Digital therapeutics, a subset of digital health, are evidence-based therapeutic interventions driven by high-quality software programs to prevent, manage, or treat a medical disorder or disease” [11].
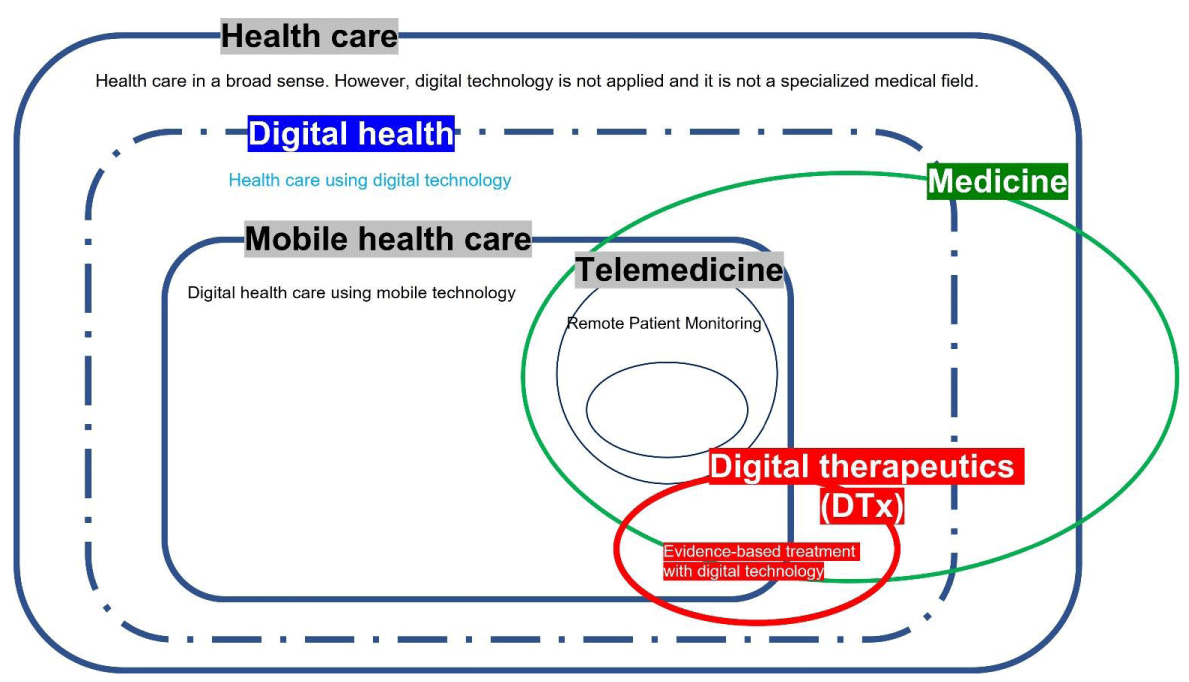
Digital therapeutics are evidenced-based, and most of them are based on behavioral correction or cognitive behavioral therapy [12]. This personal data is re-analyzed and becomes the basis for providing personalized medical care. Currently, development is actively underway in hypertension [12,13,14,15], diabetes [16], angina [17], Alzheimer’s [18], insomnia, attention deficit hyperactivity disorder (ADHD), and psychiatric disorders (depression, anxiety, abuse) [11,17,19,20] Figure 1.Figure 1: Digital health and Digital therapeutics relationship.
Among the licensed cases of digital therapy devices, the first FDA-approved digital therapy is reSET® (Pear Therapeutics Inc., Boston, USA) for the treatment of drug addiction. It was created to treat addiction to drugs such as alcohol and cocaine and was the world’s first digital therapy to be approved by the FDA in September 2017. For drug addiction treatment, the doctor prescribes reSET® to the patient, and the patient downloads a software application to input data and receive cognitive behavioral therapy. It is an example designed to fulfill the purpose and function of a typical digital therapist.
However, in the case of the current digital therapy, treatment is based on behavioral correction and monitoring. In the case of treatments that require practical and physical intervention, there is still a limit to substituting the treatment performed by the doctor at the clinic. It can be seen that there is a limit in terms of the protection of its own data so far.
Teledentistry and digital therapeutics in the dental system
Teledentistry can be developed in a way that helps to exist dental and oral diseases [2]. The first application is the remote monitoring function. In the case of the oral cavity, it has the advantage of being a part that can be accessed directly, so monitoring using a device is relatively simple. Typically, dental services can be effectively provided to patients living in rural areas. Detecting disease through early monitoring has the advantage of reducing the patient’s risk and at the same time reducing the cost. Among many studies, the function of early detection of dental caries [21], periodontitis [22] and oral cancer [23,24], using a smartphone camera is being studied. It is expected to support many parts and exert an effect with the advantage of not having to contact with the mask off in an environment that needs to reduce human-to-human contact such as COVID-19.
The second is the use of digital therapeutics that can provide behavioral correction and cognitive behavioral therapy for patients in need of treatment [25]. Many programs have been launched to improve oral hygiene by basically explaining tooth brushing and continuously evaluating its performance [26]. In addition, the introduction of digital therapeutics through cognitive behavioral therapy for pain and functional limitation or to correct bad habits in TMD patients will have an impact on areas that cannot be solved by existing medical care [4]. It is also thought to be able to function in many rehabilitation treatments, especially in the areas of simple hygiene management after various surgeries in the oral area, to assist in continuous rehabilitation treatment in the pronunciation and swallowing areas after oral cancer.
Third, medical practice using this technology is effective for data collection for future research purposes, and AI learning or cloud-based data integration can provide personalized medical care based on more accurate research [27,28].
The following forecasts should be carried out within the correct regulations and accurate research results and guidelines. Although organizations such as the USFDA have issued guidelines until recently, the pace of technological advances and unpredictable cases occur in situations such as a pandemic [29]. It should be used within the right standards and regulations that anyone can agree to in the medical field that needs to be approached conservatively.
- Shashi B. Telemedicine technologies for confronting COVID-19 pandemic: A review. Journal of Industrial Integration and Management. 2020; 5: 547-561.
- Ghai S. Teledentistry during COVID-19 pandemic. Diabetes Metab Syndr. 2020 Sep-Oct;14(5):933-935. doi: 10.1016/j.dsx.2020.06.029. Epub 2020 Jun 16. PMID: 32593116; PMCID: PMC7297180.
- Rahman N, Nathwani S, Kandiah T. Teledentistry from a patient perspective during the coronavirus pandemic. Br Dent J. 2020 Aug 14:1–4. doi: 10.1038/s41415-020-1919-6. Epub ahead of print. PMID: 32801323; PMCID: PMC7427495.
- Minervini G, Russo D, Herford AS, Gorassini F, Meto A, D'Amico C, Cervino G, Cicciù M, Fiorillo L. Teledentistry in the Management of Patients with Dental and Temporomandibular Disorders. Biomed Res Int. 2022 Apr 9;2022:7091153. doi: 10.1155/2022/7091153. PMID: 35437507; PMCID: PMC9013296.
- Abbadessa G, Lavorgna L, Miele G, Mignone A, Signoriello E, Lus G, Clerico M, Sparaco M, Bonavita S. Assessment of Multiple Sclerosis Disability Progression Using a Wearable Biosensor: A Pilot Study. J Clin Med. 2021 Mar 10;10(6):1160. doi: 10.3390/jcm10061160. PMID: 33802029; PMCID: PMC8001885.
- Lavorgna L, Iaffaldano P, Abbadessa G, Lanzillo R, Esposito S, Ippolito D, Sparaco M, Cepparulo S, Lus G, Viterbo R, Clerico M, Trojsi F, Ragonese P, Borriello G, Signoriello E, Palladino R, Moccia M, Brigo F, Troiano M, Tedeschi G, Bonavita S. Disability assessment using Google Maps. Neurol Sci. 2022 Feb;43(2):1007-1014. doi: 10.1007/s10072-021-05389-7. Epub 2021 Jun 17. Erratum in: Neurol Sci. 2021 Nov 2;: PMID: 34142263; PMCID: PMC8211455.
- Ricciardi D, Casagrande S, Iodice F, Orlando B, Trojsi F, Cirillo G, Clerico M, Bozzali M, Leocani L, Abbadessa G, Miele G, Tedeschi G, Bonavita S, Lavorgna L; Digital Technologies, Web, Social Media Study Group of the Italian Society of Neurology. Myasthenia gravis and telemedicine: a lesson from COVID-19 pandemic. Neurol Sci. 2021 Dec;42(12):4889-4892. doi: 10.1007/s10072-021-05566-8. Epub 2021 Aug 26. PMID: 34436726; PMCID: PMC8390022.
- Defining Digital Medicine. Digital Medicine Society (DiMe). Retrieved 2021-12-21.
- Join DTA.
- Kvedar JC, Fogel AL, Elenko E, Zohar D. Digital medicine's march on chronic disease. Nat Biotechnol. 2016 Mar;34(3):239-46. doi: 10.1038/nbt.3495. PMID: 26963544.
- Todd H. Digital Therapeutics Have Huge Promise And They Are Real Today. Forbes. 2015.
- Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010 Feb 17;12(1):e4. doi: 10.2196/jmir.1376. PMID: 20164043; PMCID: PMC2836773.
- Elliott WJ, Izzo JL Jr. Device-guided breathing to lower blood pressure: case report and clinical overview. MedGenMed. 2006 Aug 1;8(3):23. PMID: 17406163; PMCID: PMC1781326.
- Kario K, Nomura A, Harada N, Tanigawa T, So R, Nakagawa K, Suzuki S, Okura A, Hida E, Satake K. A multicenter clinical trial to assess the efficacy of the digital therapeutics for essential hypertension: Rationale and design of the HERB-DH1 trial. J Clin Hypertens (Greenwich). 2020 Sep;22(9):1713-1722. doi: 10.1111/jch.13993. Epub 2020 Aug 20. PMID: 32815648; PMCID: PMC7589405.
- Kario K, Nomura A, Harada N, Okura A, Nakagawa K, Tanigawa T, Hida E. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J. 2021 Oct 21;42(40):4111-4122. doi: 10.1093/eurheartj/ehab559. PMID: 34455443; PMCID: PMC8530534.
- Nordyke RJ, Appelbaum K, Berman MA. Estimating the Impact of Novel Digital Therapeutics in Type 2 Diabetes and Hypertension: Health Economic Analysis. J Med Internet Res. 2019 Oct 9;21(10):e15814. doi: 10.2196/15814. PMID: 31599740; PMCID: PMC6914106.
- Cymerys Ed; Duffy, Sean. Implementing USPSTF Recommendations on Behavioral Counseling for Cardiovascular Disease. Health Watch. 2015.
- Shuren J, Doraiswamy PM. Digital Therapeutics for MCI and Alzheimer's disease: A Regulatory Perspective - Highlights From The Clinical Trials on Alzheimer's Disease conference (CTAD). J Prev Alzheimers Dis. 2022;9(2):236-240. doi: 10.14283/jpad.2022.28. PMID: 35542995; PMCID: PMC8920745.
- Pinto MD, Greenblatt AM, Hickman RL, Rice HM, Thomas TL, Clochesy JM. Assessing the Critical Parameters of eSMART-MH: A Promising Avatar-Based Digital Therapeutic Intervention to Reduce Depressive Symptoms. Perspect Psychiatr Care. 2016 Jul;52(3):157-68. doi: 10.1111/ppc.12112. Epub 2015 Mar 19. PMID: 25800698.
- Stephanie B. Digitizing substance abuse treatment and recovery. Med City News. 2016.
- Kühnisch J, Meyer O, Hesenius M, Hickel R, Gruhn V. Caries Detection on Intraoral Images Using Artificial Intelligence. J Dent Res. 2022 Feb;101(2):158-165. doi: 10.1177/00220345211032524. Epub 2021 Aug 20. PMID: 34416824; PMCID: PMC8808002.
- Behnam A. Smartphone-Based Method for Detecting Periodontal Disease. 2019 IEEE Healthcare Innovations and Point of Care Technologies, (HI-POCT). IEEE, 2019.
- Sung-Jae L. Early detection of tongue cancer using a convolutional neural network and evaluation of the effectiveness of Efficient Net. 2022.
- Morikawa T, Kozakai A, Kosugi A, Bessho H, Shibahara T. Image processing analysis of oral cancer, oral potentially malignant disorders, and other oral diseases using optical instruments. Int J Oral Maxillofac Surg. 2020 Apr;49(4):515-521. doi: 10.1016/j.ijom.2019.08.016. Epub 2019 Sep 7. PMID: 31500953.
- Lord SE, Campbell ANC, Brunette MF, Cubillos L, Bartels SM, Torrey WC, Olson AL, Chapman SH, Batsis JA, Polsky D, Nunes EV, Seavey KM, Marsch LA. Workshop on Implementation Science and Digital Therapeutics for Behavioral Health. JMIR Ment Health. 2021 Jan 28;8(1):e17662. doi: 10.2196/17662. PMID: 33507151; PMCID: PMC7878106.
- Amantini SNSR, Montilha AAP, Antonelli BC, Leite KTM, Rios D, Cruvinel T, Lourenço Neto N, Oliveira TM, Machado MAAM. Using Augmented Reality to Motivate Oral Hygiene Practice in Children: Protocol for the Development of a Serious Game. JMIR Res Protoc. 2020 Jan 17;9(1):e10987. doi: 10.2196/10987. PMID: 31951216; PMCID: PMC6996757.
- Patel NA, Butte AJ. Characteristics and challenges of the clinical pipeline of digital therapeutics. NPJ Digit Med. 2020 Dec 11;3(1):159. doi: 10.1038/s41746-020-00370-8. PMID: 33311567; PMCID: PMC7733514.
- Wiederhold BK. Data-Driven Digital Therapeutics: The Path Forward. Cyberpsychol Behav Soc Netw. 2021 Oct;24(10):631-632. doi: 10.1089/cyber.2021.29227.editorial. Epub 2021 Sep 22. PMID: 34551264.
- Guidance with Digital Health Content. USFDA.