More Information
Submitted: March 24, 2023 | Approved: June 01, 2023 | Published: June 02, 2023
How to cite this article: Yadav J, Shinh AS, Natt AS, Maheshwari K, Aulakh S. Oral hygiene status: The critical parameter in orthodontic patient. J Clin Adv Dent. 2023; 7: 007-012.
DOI: 10.29328/journal.jcad.1001034
Copyright License: © 2023 Yadav J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Oral hygiene; Fixed orthodontic mechanotherapy; Gingivitis
Oral hygiene status: The critical parameter in orthodontic patient
Jyoti Yadav*, Amanish Singh Shinh, Amanpreet Singh Natt, Karan Maheshwari and Sharnjeet Aulakh
Adesh Institute of Dental Sciences & Research, Bathinda, Punjab, India
*Address for Correspondence: Jyoti Yadav, Adesh Institute of Dental Sciences & Research, Bathinda, Punjab, India, Email: [email protected]
Aim: The aim of this study was to evaluate the oral hygiene status of patients with fixed mechanotherapy appliances.
Methods and materials: The following indices were used to evaluate the oral hygiene status of patients in orthodontic treatment: Gingival Bleeding Index (GBI), Plaque index (PI) and OrthoPlaque Index (OPI) at three intervals.T0 (day 1), T1 (15 days), T2 (30 days) for a period of one month.
Results: 10 patients (15-30 years old) were selected for the study from among the orthodontic patients treated at the Department of Orthodontics & Dentofacial Orthopedics, AIDSR, Adesh University. Results showed that the mean PI decreased significantly from T0 to T1 & then from T1 to T2, GI decreased significantly from T0 to T1, but then, no significant difference could be found in GI from T1 to T2, OPI decreased significantly from T0 to T1, but then, no significant difference could be found in OPI from T1 to T2. No significant difference was observed between male and female patients for the PI, GI and OPI.
Conclusion: Inadequate oral home care among orthodontic patients may increase their risk of gingivitis during treatment. As a result, oral hygiene instructions and a hygiene maintenance program must not be overlooked during orthodontic treatment.
Adult patients are increasingly seeking orthodontic treatment in modern dental care. Following the placement of fixed orthodontic appliances, oral hygiene becomes significantly more difficult [1-3]. As a result, patients wearing fixed orthodontic appliances are more likely to develop dental caries and gingivitis, which can lead to gingival attachment loss [4]. After three months of active orthodontic treatment, there is a statistically significant increase in stimulated salivary flow rate, pH, buffer capacity, plaque index (PLI) scores, and lactobacilli levels [5,6]. Differences in the plaque index (PI), bleeding index (BI), and pocket depth (PD) measures were found following the placement of fixed appliances, and these values were significantly greater than the baseline [7,8]. A shift to a more disease-inducing subgingival microflora was reported, with a statistically significant increase in spirochetes and fusiform bacilli. A significant change in oral microbiota was found in subjects with fixed appliances during the first six months of treatment [9,10]. Such a result suggests that the risk of gingivitis was high during their months of therapy, and the risk of periodontitis could not be ruled out. Manschot [11] described a patient who had severe mucogingival changes, such as gingival recession, as a result of orthodontic treatment and poor oral hygiene [12]. Orthodontic appliances do not usually cause gingival inflammation, but the increase in microorganisms can contribute to periodontal disease [13]. Plaque accumulation and gingival inflammation, on the other hand, can both be reduced in motivated patients [14,15].
As a result, it is critical to emphasize oral hygiene instructions to orthodontic patients who are wearing a fixed appliance [16].
The purpose of this study was to assess the level of oral hygiene in patients receiving fixed orthodontic appliances.
Ethical clearance
Ethical clearance was approved by the Ethical Committee of Adesh University before conducting the present study with letter number AU/CoE/MDS/05/17 dated 22/12/21.
Patients undergoing fixed mechanotherapy were selected randomly from the Department of Orthodontics and Dentofacial Orthopedics, AIDSR, Adesh University.
Patients in fixed mechanotherapy in the orthodontic department at Adesh Institute of Dental Sciences & Research, Bathinda were chosen for the study.
The study was conducted by one investigator so no inter-operator bias was present.
Inclusion criteria
1. Patients with full-mouth fixed orthodontic appliances that had been in place for at least six months.
2. No systemic diseases.
3. No history of taking antibiotics for the last three months.
4. No oral prophylaxis during the month preceding the study.
Exclusion criteria
1. Nonorthodontic patients.
2. Patients having systemic diseases.
3. Patients have a history of taking antibiotics for the last three months.
Orthodontic Plaque Index (OPI): Gingival Bleeding Index (GBI) & The Plaque Index (PI) were used to evaluate the patient’s oral hygiene and the gingiva. The Orthodontic Plaque Index (OPI) [17] was used to assess plaque levels in the most critical plaque accumulation zones, which are cervical to the bracket base and mesial and distal to the bracket body. The index formula shown in Table 1 was used to calculate OPI.
| Table 1: Orthodontic Plaque Index [17]. | |
| Score | Criteria |
| 0 | No plaque deposits on the tooth surfaces surrounding the bracket base |
| 1 | Plaque deposits on 1 tooth surface at the bracket base. |
| 2 | Plaque deposits on 2 tooth surfaces at the bracket base. |
| 3 | Plaque deposits on 3 tooth surfaces at the bracket base. |
| 4 | Plaque deposits on 4 tooth surfaces at the bracket base and gingival |
Gingival Index (GI): To calculate the gingival bleeding index (GI) [3], all four surfaces of the teeth were examined to see if probing caused bleeding. The severity of gingivitis was determined using the score shown in Table 2 [3].
| Table 2: Gingival Index [3]. | |
| Score | Criteria |
| 0 | Normal gingiva |
| 1 | Mild inflammation - a slight change in color and slight edema but no bleeding on probing |
| 2 | Moderate inflammation - redness, edema, glazing, bleeding on probing. |
| 3 | Severe inflammation marked redness and edema, ulceration with a tendency to spontaneous bleeding. |
| Table 3: Gingival Index. | |
| Score | Criteria |
| 0 | No plaque |
| 1 | Thin plaque layer at the gingival margin, only detectable by scraping with a probe |
| 2 | A moderate layer of plaque along the gingival margin, interdental spaces are free, but plaque is visible to the naked eye |
| 3 | Abundant plaque along the gingival margin, interdental spaces filled with plaque |
Data analysis
Data was entered into the computer using the FoxPro program [FoxPro 7.0; Sybase Inc., Dublin, CA, USA] and statistical analyses were performed using the Statistical Package for the Social Sciences [SPSS 10; (SPSS Inc., Chicago, IL, USA)]. To determine differences at the 5% significance level (p0.05), a one-way analysis of variance (ANOVA) was used.
The mean age of male & female study participants was found to be comparable Tables 4,5.
| Table 4: Descriptives of Age of the study participants. | ||||
| sex | N | Mean | Std. Deviation | |
| Age | Males | 4 | 19.25 | 4.425 |
| Females | 6 | 20.00 | 2.898 | |
| Table 5: Intragroup comparison of Mean Plaque Index at T0, T1 & T2. | |||||
| Plaque Index | |||||
| N | Minimum | Maximum | Mean | Std. Deviation | |
| T0 | 10 | .80 | 2.00 | 1.5320 | .39454 |
| T1 | 10 | .50 | 1.50 | 1.0820 | .39355 |
| T2 | 10 | .3 | 1.0 | .570 | .1767 |
| p value | < 0.001, S | ||||
| Post hoc Pairwise comparison | T0 > T1 > T2 | ||||
Intragroup comparison of the Mean Plaque Index at T0, T1 & T2 was done using the Friedman test. A statistically significant difference was found in the mean PI score at T0, T1 & T2. Post hoc pairwise comparison was done using the Wilcoxon test. It was found that the mean PI decreased significantly from T0 to T1 & then from T1 to T2 Table 6.
| Table 6: Intragroup comparison of Mean Gingival Index at T0, T1 & T2. | |||||
| Gingival Index | |||||
| N | Minimum | Maximum | Mean | Std. Deviation | |
| T0 | 10 | .60 | 1.50 | 1.0060 | .30826 |
| T1 | 10 | .5 | .6 | .540 | .0516 |
| T2 | 10 | .16 | .60 | .3760 | .13818 |
| p value | < 0.001, S | ||||
| Post hoc Pairwise comparison | T0 > T1, T2 | ||||
Intragroup comparison of the Mean Gingival Index at T0, T1 & T2 was done using the Friedman test. A statistically significant difference was found in the mean GI score at T0, T1 & T2. Post hoc pairwise comparison was done using the Wilcoxon test. It was found that the mean GI decreased significantly from T0 to T1, but then, no significant difference could be found in GI from T1 to T2 Table 7.
| Table 7: Intragroup comparison of Mean OPI at T0, T1 & T2. | |||||
| Ortho Plaque Index | |||||
| N | Minimum | Maximum | Mean | Std. Deviation | |
| T0 | 10 | 2 | 3 | 2.70 | .483 |
| T1 | 10 | 1 | 2 | 1.60 | .516 |
| T2 | 10 | 1 | 2 | 1.20 | .422 |
| P value | <0.001 | ||||
| Post hoc Pairwise comparison | T0 > T1 >T2 | ||||
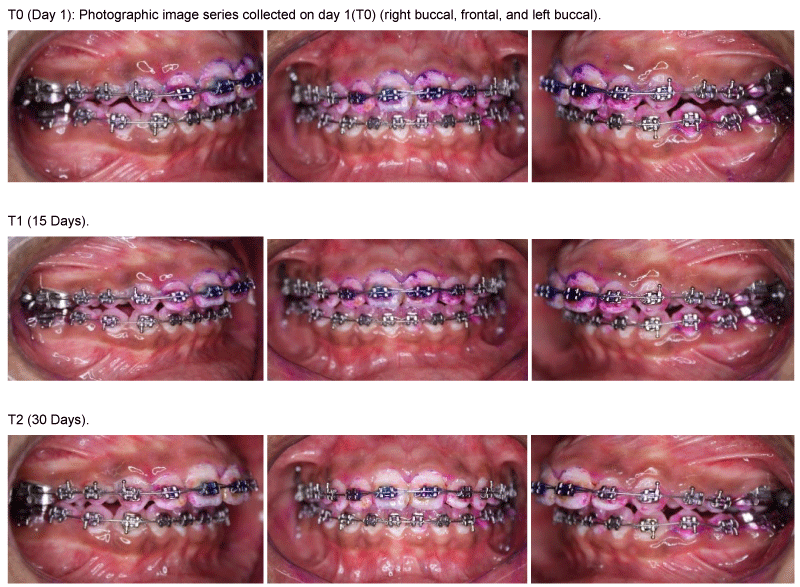
Intragroup comparison of Mean OPI at T0, T1 & T2 was done using the Friedman test. A statistically significant difference was found in the mean OPI score at T0, T1 & T2. Post hoc pairwise comparison was done using the Wilcoxon test. It was found that the mean OPI decreased significantly from T0 to T1, but then, no significant difference could be found in OPI from T1 to T2 Figure 1.
Figure 1: At T0, TI (15 days), T1 (30 days).
Because of the increased challenge to oral hygiene, patients undergoing orthodontic treatment with fixed appliances are at risk for developing gingival inflammation. Gingivitis is caused primarily by dental plaque [18,19]. The inability of the patient to adequately clean his or her teeth around fixed orthodontic devices promotes plaque accumulation, which can then lead to gingival inflammation. After orthodontic appliance placement, there is an overall increase in salivary bacterial counts, particularly Lactobacillus [20,21]. Similarly, twofold and threefold increases in clinical indexes and motile organism numbers have been reported six months after appliance placement [2], as well as an early increase in anaerobes and Prevotella intermedia and a decrease in facultative anaerobes [3,22]. This shift in subgingival microflora to a periopathogenic population is comparable to the microflora found in periodontally diseased sites [23,24]. Plaque control may be made more difficult by irregular tooth alignment. Some studies have discovered a link between crowding and periodontal disease [25], while others have not [26,27]. Nonetheless, effective plaque control is the most important factor in maintaining good oral hygiene [28]. The purpose of this study was to assess oral hygiene among orthodontic patients at Adesh Institute of Dental Sciences & Research. Despite the fact that more than half of the patients brush their teeth twice a day, their oral hygiene was poor. In general, PI and OPI were reduced after oral prophylaxis, with mean values of 1.5 to 0.5 and 2.7-1.2, respectively. This finding is consistent with previous research that found an increase in visible plaque on tooth surfaces following the placement of orthodontic appliances [25,26,29]. This is due to an increase in plaque retentive areas as well as the patient’s inability to perform adequate oral hygiene [30]. However, increasing the frequency of brushing does not guarantee clean teeth. As a result, toothbrushing frequency alone cannot be used to assess the quality of oral hygiene [31-34].
Education and motivation, as well as continuous reinforcement of oral hygiene, can improve patients’ oral home care performance. Orthodontic patients, in particular, must be educated on proper oral hygiene maintenance, and their brushing habits must be monitored on a regular basis. Following an intensive period of individual oral hygiene education, it is possible to achieve and maintain a high standard of oral health behavior [35]. When evaluating the brushing techniques used, it is clear that patients require motivation and instruction on how to use an appropriate technique. Previously, the so-called scrubbing method was recommended to patients during orthodontic treatment; however, the modified Bass technique outperformed the scrub method [36]. Many patients place the toothbrush too far coronally, ignoring the gingival third of the tooth, which can lead to increased plaque accumulation and the development of gingivitis. As a result, all patients should be instructed to clean both the tooth structure cervical to an orthodontic appliance and the remaining coronal surfaces [37]. In the presence of orthodontic appliances, some patients may find daily oral hygiene difficult. As a result, patients with orthodontic appliances should use an electric toothbrush. Indeed, Heintze, et al. [17] concluded that patients with poor oral hygiene may benefit from using an electric toothbrush, particularly because dental plaque can be easily and quickly removed. Electric toothbrushes with a rotational brush are significantly more effective than manual toothbrushes in removing supragingival plaque from bracketed teeth. In fact, differences in plaque-removing effectiveness were discovered to be especially consistent on the proximal surfaces of teeth [38]. According to the findings of this study, the majority of the patients (68 percent) did not visit a dental hygienist during their orthodontic treatment. Professional prophylaxis has been shown to be effective in patients with fixed orthodontic appliances [39]. As a result, oral hygiene instruction and reinstruction are required during orthodontic treatment. Some patients should also be reminded to clean the cervical area of their teeth below the brackets. Increased oral hygiene awareness will not only reduce the prevalence and severity of iatrogenic tissue damage but will also extend the long-term benefits of orthodontic therapy [40].
The mean GBI value was reduced from 1.0 to 0.3, which is regarded as a reasonable value. The results of this study revealed that the relationship between the three indices and gender was not significant for the PI and OPI, but significant for the GBI (p = 0.05) [41].
According to the findings of this study, patients wearing orthodontic appliances have difficulty maintaining good oral hygiene. As a result, educating and motivating these patients to maintain their oral health, as well as recommending oral home care aids to improve compliance, remains the cornerstone for achieving optimal oral hygiene results.
Patients must understand what their treatment will entail and what their responsibilities will be. They must understand that they are partners in their orthodontic treatment and that they have the opportunity to improve and then maintain good oral health.
No oral hygiene program, however, will be successful unless orthodontists accept responsibility for motivating their patients and staff. When an orthodontist offers oral hygiene advice with genuine interest and respect, patients usually respond positively and become receptive to self-improvement. As a result, any hygiene issues or limitations discovered during orthodontic treatment must not be ignored but must be addressed right away.
Clinical significance
Inadequate oral home care among orthodontic patients may increase their risk of gingivitis during orthodontic treatment. It is therefore critical that proper oral hygiene be maintained throughout orthodontic treatment.
Limitations
The limitation of the present study was that the sample size was small, and the results may not be significant or representative in nature.
- Zachrisson S, Zachrisson BU. Gingival condition associated with orthodontic treatment. Angle Orthod. 1972 Jan;42(1):26-34. doi: 10.1043/0003-3219(1972)042<0026:GCAWOT>2.0.CO;2. PMID: 4500561.
- Leggott PJ, Boyd RL, Quinn RS, Eakle WS, Chambers DW. Gingival disease pattern during fixed orthodontic therapy adolescents versus adults. J Dent Res. 1984; 63 (Special issue): 309, abstract 1245.
- Huser MC, Baehni PC, Lang R. Effects of orthodontic bands on microbiologic and clinical parameters. Am J Orthod Dentofacial Orthop. 1990 Mar;97(3):213-8. doi: 10.1016/S0889-5406(05)80054-X. PMID: 2309668.
- Zachrisson BU, Alnaes L. Periodontal condition in orthodontically treated and untreated individuals. I. Loss of attachment, gingival pocket depth and clinical crown height. Angle Orthod. 1973 Oct;43(4):402-11. doi: 10.1043/0003-3219(1973)043<0402:PCIOTA>2.0.CO;2. PMID: 4517973.
- Chang HS, Walsh LJ, Freer TJ. The effect of orthodontic treatment on salivary flow, pH, buffer capacity, and levels of mutans streptococci and lactobacilli. Aust Orthod J. 1999 Apr;15(4):229-34. PMID: 11933357.
- Paolantonio M, Pedrazzoli V, di Murro C, di Placido G, Picciani C, Catamo G, De Luca M, Piaccolomini R. Clinical significance of Actinobacillus actinomycetemcomitans in young individuals during orthodontic treatment. A 3-year longitudinal study. J Clin Periodontol. 1997 Sep;24(9 Pt 1):610-7. doi: 10.1111/j.1600-051x.1997.tb00237.x. PMID: 9378831.
- Marini I, Bortolotti F, Parenti SI, Gatto MR, Bonetti GA. Combined effects of repeated oral hygiene motivation and type of toothbrush on orthodontic patients: a blind randomized clinical trial. Angle Orthod. 2014 Sep;84(5):896-901. doi: 10.2319/112113-856.1. Epub 2014 Mar 18. PMID: 24641783; PMCID: PMC8641274.
- Kapoor D, Gill S, Singh A, Kaur I, Kapoor P. Oral hygiene awareness and practice amongst patients visiting the Department of Periodontology at a Dental College and Hospital in North India. Indian J Dent. 2014 Apr;5(2):64-8. doi: 10.4103/0975-962X.135262. PMID: 25565727; PMCID: PMC4184328.
- Petti S, Barbato E, Simonetti D'Arca A. Effect of orthodontic therapy with fixed and removable appliances on oral microbiota: a six-month longitudinal study. New Microbiol. 1997 Jan;20(1):55-62. PMID: 9037669.
- Pinto AS, Alves LS, Zenkner JEDA, Zanatta FB, Maltz M. Gingival enlargement in orthodontic patients: Effect of treatment duration. Am J Orthod Dentofacial Orthop. 2017 Oct;152(4):477-482. doi: 10.1016/j.ajodo.2016.10.042. PMID: 28962731.
- Manschot A. Orthodontics and inadequate oral hygiene compliance as a combined cause of localized gingival recession: a case report. Quintessence Int. 1991 Nov;22(11):865-70. PMID: 1812508.
- Jadhav T, Bhat KM, Bhat GS, Varghese JM. Chronic inflammatory gingival enlargement associated with orthodontic therapy--a case report. J Dent Hyg. 2013 Feb;87(1):19-23. Epub 2013 Feb 5. PMID: 23433694.
- Parker RB. Our common enemy. J Am Soc Prev Dent. 1971 Jan-Feb;1(2):14-7 passim. PMID: 5279779.
- Axelsson P. Needs-related plaque control measures based on risk prediction. A. R. In: Lang PN, Attström R, Löe H, editors. Proceedings of the European Workshop on Mechanical Plaque Control. Chicago: Quintessence Publishing; 1998; 190-247.
- Ajayi EO, Azodo CC. Oral hygiene status among orthodontic patients attending university of Benin Teaching Hospital, Benin city, Nigeria. J Dent Health Oral Disord Ther. 2014;1(4):23.
- Zhao H, Xie Y, Meng H. [Effect of fixed appliance on periodontal status of patients with malocclusion.] Zhonghua Kou Qiang Yi Xue Za Zhi. 2000; 35(4):286-8.
- Heintze SD, Jost-Brinkmann PG, Finke C, Miethke RR. Ortho-plaque Index. In: Oral health for the orthodontic patient. Chicago: Quintessence; 1999; 67-70.
- Loe H, Theilade E, Jensen SB. Experimental Gingivitis in Man. J Periodontol (1930). 1965 May-Jun;36:177-87. doi: 10.1902/jop.1965.36.3.177. PMID: 14296927.
- Khoroushi M, Kachuie M. Prevention and Treatment of White Spot Lesions in Orthodontic Patients. Contemp Clin Dent. 2017 Jan-Mar;8(1):11-19. doi: 10.4103/ccd.ccd_216_17. PMID: 28566845; PMCID: PMC5426141.
- Bloom RH, Brown LR. A study of the effects of orthodontic appliances on the oral microbial flora. Oral Surg Oral Med Oral Pathol. 1964 May;17:658-67. doi: 10.1016/0030-4220(64)90373-1. PMID: 14131587.
- Muntean A, Sava S, Delean AG, Mihailescu AM, Dumitrescu LS, Moldovan M, Festila DG. Toothpaste Composition Effect on Enamel Chromatic and Morphological Characteristics: In Vitro Analysis. Materials (Basel). 2019 Aug 16;12(16):2610. doi: 10.3390/ma12162610. PMID: 31426296; PMCID: PMC6720655.
- Diamanti-Kipioti A, Gusberti FA, Lang NP. Clinical and microbiological effects of fixed orthodontic appliances. J Clin Periodontol. 1987 Jul;14(6):326-33. doi: 10.1111/j.1600-051x.1987.tb00979.x. Erratum in: J Clin Periodontol 1990 Jan;17(1):66. PMID: 3509967.
- Peng Y, Wu R, Qu W, Wu W, Chen J, Fang J, Chen Y, Farella M, Mei L. Effect of visual method vs plaque disclosure in enhancing oral hygiene in adolescents and young adults: a single-blind randomized controlled trial. Am J Orthod Dentofacial Orthop. 2014 Mar;145(3):280-6. doi: 10.1016/j.ajodo.2013.10.021. PMID: 24582019.
- Rose J, Ghoneima A, Lippert F, Maxwell L, Eckert G, Stewart KT. A visual evaluation of oral plaque removal utilizing an adjunct enzyme pre-rinse in orthodontic subjects. Angle Orthod. 2020 Nov 1;90(6):844-850. doi: 10.2319/120819-776.1. PMID: 33378520; PMCID: PMC8028437.
- Buckley LA. The relationship between malocclusion and periodontal disease. J Periodontol. 1972 Jul;43(7):415-7. doi: 10.1902/jop.1972.43.7.415. PMID: 4504525.
- Geiger AM, Wasserman BH, Turgeon LR. Relationship of occlusion and periodontal disease. 8. Relationship of crowding and spacing to periodontal destruction and gingival inflammation. J Periodontol. 1974 Jan;45(1):43-9. doi: 10.1902/jop.1974.45.1.43. PMID: 4520353.
- Saruttichart T, Chantarawaratit PO, Leevailoj C, Thanyasrisung P, Pitiphat W, Matangkasombut O. Effectiveness of a motionless ultrasonic toothbrush in reducing plaque and gingival inflammation in patients with fixed orthodontic appliances. Angle Orthod. 2017 Mar;87(2):279-285. doi: 10.2319/042516-334.1. Epub 2016 Sep 19. PMID: 27636178; PMCID: PMC8384361.
- Listgarten MA, Helldén L. Relative distribution of bacteria at clinically healthy and periodontally diseased sites in humans. J Clin Periodontol. 1978 May;5(2):115-32. doi: 10.1111/j.1600-051x.1978.tb01913.x. PMID: 350909.
- Lundström F, Hamp SE, Nyman S. Systematic plaque control in children undergoing long-term orthodontic treatment. Eur J Orthod. 1979;2(1):27-39. PMID: 296948.
- Hamp SE, Lundström F, Nyman S. Periodontal conditions in adolescents subjected to multiband orthodontic treatment with controlled oral hygiene. Eur J Orthod. 1982 May;4(2):77-86. doi: 10.1093/ejo/4.2.77. PMID: 6955179.
- Buthelezi NL, Madiba TK. Oral hygiene habits and status of orthodontic patients attending the University of Pretoria, Oral and Dental Hospital. South African Dental Journal. 2021; Apr;76(3):130-5.
- Chhibber A, Agarwal S, Yadav S, Kuo CL, Upadhyay M. Which orthodontic appliance is best for oral hygiene? A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2018 Feb;153(2):175-183. doi: 10.1016/j.ajodo.2017.10.009. PMID: 29407494.
- Ajayi EO, Azodo CC. Oral hygiene status among orthodontic patients attending university of Benin Teaching Hospital, Benin city, Nigeria. J Dent Health Oral Disord Ther. 2014; 1(4):23.
- Eppright M, Shroff B, Best AM, Barcoma E, Lindauer SJ. Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod. 2014 Mar;84(2):208-13. doi: 10.2319/062813-481.1. Epub 2013 Sep 12. PMID: 24028316; PMCID: PMC8673795.
- Wites M, Panuszka J, Dyras M. Ocena higieny jamy ustnej i aparatów regulacyjnych u pacjentów leczonych ortodontycznie [Evaluation of oral and orthodontic appliance hygiene in orthodontically treated patients]. Przegl Lek. 2003;60 Suppl 6:126-8. Polish. PMID: 15106476.
- Björn H, Lindhe J. On the mechanics of toothbrushing. Odontol Revy. 1966;17(1):9-16. PMID: 5218905.
- Pinto AS, Alves LS, Zenkner JEDA, Zanatta FB, Maltz M. Gingival enlargement in orthodontic patients: Effect of treatment duration. Am J Orthod Dentofacial Orthop. 2017 Oct;152(4):477-482. doi: 10.1016/j.ajodo.2016.10.042. PMID: 28962731.
- Trombeli L, Scabbia A, Griselli A, Zangari F, Calura G. Clinical evaluation of plaque removal by counterrotational electric toothbrush in orthodontic patients. Quintessence Int. 1995 Mar;26(3):199-202. PMID: 7568736.
- Alstad S, Zachrisson BU. Longitudinal study of periodontal condition associated with orthodontic treatment in adolescents. Am J Orthod. 1979 Sep;76(3):277-86. doi: 10.1016/0002-9416(79)90024-1. PMID: 290273.
- Public Health England. Delivering Better Oral Health:An Evidence-based Toolkit for Prevention, 3rd edn. London: PHE, 2017.
- Carlsson J, Egelberg J. Effect of diet on early plaque formation in man. Odontol Revy. 1965;16:112-25. PMID: 14308499.
- O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972 Jan;43(1):38. doi: 10.1902/jop.1972.43.1.38. PMID: 4500182.
- Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975 Dec;25(4):229-35. PMID: 1058834.
- Waerhaug J. The interdental brush and its place in operative and crown and bridge dentistry. J Oral Rehabil. 1976 Apr;3(2):107-13. doi: 10.1111/j.1365-2842.1976.tb00934.x. PMID: 1066443.
- Krishnan V, Ambili R, Davidovitch ZE, Murphy NC. Gingiva and orthodontic treatment. In Seminars in Orthodontics 2007; (Vol. 13, No. 4: 257-271). WB Saunders