More Information
Submitted: October 16, 2023 | Approved: November 02, 2023 | Published: November 03, 2023
How to cite this article: Zeroual R, Bahedi O. The Use of Polyetheretherketone (PEEK) in Implant Prosthetics: A Detailed Review of the Literature. J Clin Adv Dent. 2023; 7: 034-040.
DOI: 10.29328/journal.jcad.1001038
Copyright License: © 2023 Zeroual R, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: PEEK; Polyetheretherketone; Prosthetics; Dental implant
The Use of Polyetheretherketone (PEEK) in Implant Prosthetics: A Detailed Review of the Literature
Rajae Zeroual* and Oussama Bahedi
Department of Removable Prosthodontics, Faculty of Dentistry, Hassan II University, Casablanca, Morocco
*Address for Correspondence: Rajae Zeroual, Department of Removable Prosthodontics, Faculty of Dentistry, Hassan II University, Casablanca, Morocco, Email: [email protected]
Background: The aim of this review is to discuss the properties of PEEK, its implant applications and its prosthetic interest compared to other materials currently used in dentistry.
Methods: The data was searched through PubMed database, Science Direct-Elsevier and Google scholar by several keywords in various combinations with a time period 2012-2023. Unavailable in full text, non-English, non-French data were excluded, as well as studies that do not meet the objectives of the study.
Results: The articles were of various nature and were filtered after eliminating duplicates, reading the title, summary and full text. Of the 1673 articles selected, 51 were deemed relevant. The selected studies and clinical trials were detailed in tables.
Conclusion: Due to its superior mechanical, biological and aesthetic properties, PEEK appears to be a promising alternative to titanium and its alloys. However, further in vivo research is still needed to determine if PEEK can completely replace titanium and other implant materials in the future.
One of the challenges of modern dentistry is to improve the biomechanical and biocompatible properties of materials used for implant treatment [1]. Dental implants improve the quality of life of many patients who have lost their teeth. The material of choice for oral endosseous implants is pure titanium, introduced in the late 1960s by Branemark [2].
However, titanium can cause aesthetic problems due to its lack of light transmission. This can cause a dark reflection of the peri-implant soft tissue in cases of thin biotype mucosa and/or mucosal recession around a titanium implant. This can be problematic, especially in the presence of a high smile line [2].
The increasing demand for metal-free materials in dentistry, as well as the increase in sensitivity and allergies, has spurred advances in materials science. About 40 years ago, aluminum oxide ceramic implants were proposed as a replacement for titanium. However, this material could not meet the standards because of the high incidence of fractures [3].
Recently, PEEK has gained increasing interest as an alternative to titanium due to its high biocompatibility, preferred color, economical price, and chairside adjustability [4].
PEEK is a semi-crystalline aromatic polycyclic thermoplastic polymer that has been used in orthopedic surgery since the 1990s because its mechanical and physical properties resemble those of bone [4]. It is used in implant dentistry, including dental implants, temporary abutments, temporary crowns on implants, fixed prostheses and removable dental prostheses [5].
It is a material with high biocompatibility, good mechanical properties, resistance to high temperatures, chemical stability, polishability, good wear resistance, low affinity to plaque and high bond strength to veneering composites and cements [6].
The purpose of this literature review was to present PEEK as a material and its properties, research all the prosthetic implant applications of PEEK available in the literature and demonstrate the prosthetic interest of PEEK compared to the materials currently used in dentistry.
The aim of this review is to answer the main research question: What are the properties and the prosthetic applications of polyetheretherketone?
To answer this question, we adopted an electronic search strategy based on a systemic query of 3 databases: PubMed, Science Direct and Google Scholar. Searches were conducted using relevant predefined keywords and MeSH terms such as “PEEK”, “Polyetheretherketone”, “Prosthetics”, “Dental implant”. These keywords were used in multiple combinations and equations using Boolean operators “AND”, “OR”, to create the search string for studies’ titles and abstracts.
The articles included in the search were articles: meeting the objectives of the study and published between 2012 and 2023. We excluded publications written in languages other than French or English and articles unavailable in full text.
Study selection process and flow chart
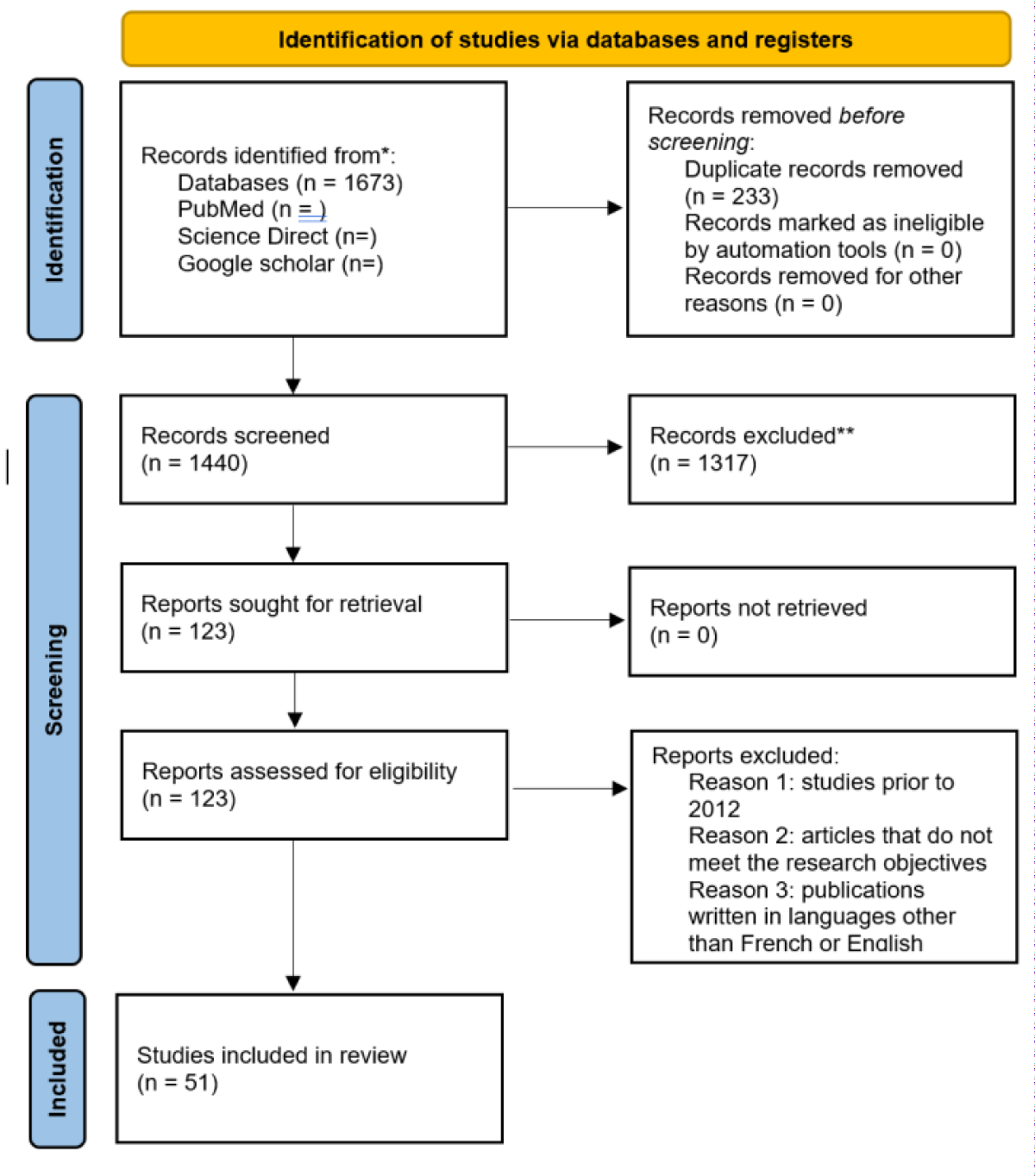
Using the 3 search engines: PubMed, Science Direct and Google scholar, our strategy identified 1673 articles. Of these 1673 articles, 233 were eliminated as they were duplicates. Among the remaining 1440 articles, a first reading based on titles and abstracts was performed for pre-selection purposes. This screening allowed the elimination of 1317 articles that were not directly related to the subject. Of the 123 articles retained, a third level of screening, consisting of a critical reading of the full-text articles, allowed us to retain 51 articles that met the research objectives. In the end, 51 articles were included as relevant to our research (Figure 1).
Figure 1: Flow Chart as per PRISMA.
Analysis of selected articles
The bibliographic search was conducted in English and French on 3 different search engines. A total of 51 studies were included in our review: 19 in vitro studies, 3 case reports and 29 literature reviews.
Biological properties of peek
Biocompatibility: Overall, PEEK has decent biocompatibility. According to Yin, et al. [7]. PEEK has no cytotoxicity and would not cause cell mutation, indicating low cytotoxicity and genotoxicity, but it still has some limitations. One of the main problems is the chemical and biological inertia of PEEK biomaterials. Another problem is the very hydrophobic surface. These two factors do not allow either protein absorption or cell adhesion.
Osseointegration: The bioinert properties and highly hydrophobic surface of PEEK generally result in poor osseointegration and limited initial fixation and long-term stability of the implant, as it cannot form a bone bond with the host bone tissue. In addition, they do not allow protein uptake or cell adhesion [7]. A study comparing titanium, PEEK, and zirconia as implant materials found that PEEK had the lowest bone contact with the implant (2). Recent efforts have focused on increasing the bioactivity of PEEK by impregnating bioactive materials into the PEEK substrate [8].
Allergenic potential: PEEK is an inert material. All the studies reviewed show that it is non-allergenic and has a low affinity for dental plaque [6,9,10].
Antibacterial potential: It has been shown that chemical composition, surface kinetic energy and surface roughness are able to affect bacterial adhesion [11]. In terms of surface roughness, Barkarmo, et al. [12] compared biofilm formation on polished and sandblasted PEEK. They found that sandblasted PEEK with a rougher surface topography had an increased number of bacteria, with the bacteria observed including Streptococcus sanguinis, Streptococcus oralis, and Streptococcus gordonii. Regarding the chemical composition, research by D’Ercole, et al. [13] has already proven that, compared to titanium, PEEK showed anti-adhesive and antibacterial properties between 24 and 48 hours against oral bacteria such as Streptococcus oralis.
Mechanical properties of peek
Density: The density of material is the ratio of its density to the density of pure water. For the polymer family, density is considered the specific gravity of the biomaterial and is expressed in g/cm3. PEEK has a density of 1.3 g/cm3 and a thermal conductivity of 0.29 W/mK [6].
Modulus of elasticity: The modulus of elasticity of the implant material has an influence on the healing process, success and survival rate of the implant under different loading conditions. A modulus of elasticity close to that of bone optimizes the biomechanical load distribution between the implant and the surrounding bone and maintains the bone-implant contact [8]. One of the most important properties of PEEK is the Young’s modulus. The Young’s modulus of PEEK is 3 - 4 GPa and can be easily modified by adding carbon fibers or ceramic particles to increase the values to 18 GPa close to that of trabecular bone (10 - 14 GPA) and cortical bone (18 - 20 GPA) [4,8,14].PEEK will therefore exhibit better shock absorption capacity than other materials such as titanium, which has a much higher modulus of elasticity, ranging from 102 to 110 GPa [9].
Tensile and flexural strength: The tensile strength of PEEK is 80 MPa and up to 120 MPa when modified (BioHPP), which is comparable to dentin (104 MPa) and enamel (46.5 MPa), while titanium is 954 - 976 MPa and zirconia is 1000 MPa, thus making it a suitable restorative material in terms of mechanical properties [4].
Material wear: The balanced wear resistance of PEEK can be matched by very few polymers [15]. Irregularities in the counter surface cause abrasive wear during cutting, while repeated stresses and pressures cause deformation of the material resulting in fatigue wear. The resistive force that opposes movement is called friction. The negative effects of fatigue and abrasion wear as well as friction are overcome by the properties of PEEK due to its resistive nature and low friction coefficient [15]. Liebermann, et al. [16] evaluated the effects of aging on several materials (PEEK, PMMA, composite resin, hybrid materials) and showed that PEEK had the lowest solubility and water absorption values.
However, the mechanical properties of PEEK are affected by temperature changes, which show dramatic decreases when the temperature reaches 250 °C. In particular, when the temperature is higher than 150 °C (i.e., when it exceeds the transition temperature of glass), the mechanical properties show a significant decrease [2].
Peek applications in implantology
PEEK was first introduced into dental applications in 1992, first as aesthetic abutments and then as implants. Subsequently, it has been successfully used as a material in a number of applications, including dental implants, healing abutments, temporary abutments (due to its mechanical strength, aesthetic qualities, soft tissue response, and ability to shape easily) and implant-supported prostheses [17,18].
The iso-elasticity of PEEK composites allows them to deform identically to bone and thus produce a more homogeneous stress distribution along the implant-bone interface. They have shown good strength, fracture toughness and satisfactory bio-inertia [17].
Abutments
Metals such as titanium and ceramics such as zirconium oxide are used for dental implant abutments. Recently, PEEK has been introduced as a restorative material in implant dentistry and is increasingly used as an implant abutment material [19]. PEEK abutments have lower biofilm formation on their surface than traditional abutment materials and promote the bone remodeling process [3].
They are suitable for long-term provisional restorations, especially in the anterior region. Their limitations are high vertical displacement, plastic deformation, high torque loss, microleakage and low fracture resistance [2,20]. Because of the semicrystalline structure of PEEK, which reduces brittleness, deformation rather than fracture is observed. Therefore, PEEK abutments can be changed simply when needed, avoiding the need to remove a broken screw, which is often the case with titanium abutments [3].
In a study by Ortega-Martinez, et al. [21], titanium implant abutments were better than PEEK abutments in all mechanical tests. The strength loss of the titanium abutments was approximately 10%, whereas PEEK had a significantly higher strength loss of up to 50%. In addition, 91.6% of the titanium abutments did not show microleakage, while none of the PEEK abutment specimens showed microleakage when subjected to dynamic loading.
Regarding the fracture resistance of resin-on-implant crowns, no significant difference was observed between PEEK and temporary titanium abutments, except for the central incisors, as reported by Santing, et al. [18].
In summary, there are only a few studies on the clinical evaluation of PEEK abutments, and the longest research studies lasted only a few months. Further clinical trials are needed to evaluate hard and soft tissue responses to PEEK materials and their reduced biofilm formation.
Abutments screws
The advantages given by PEEK abutment screws are related to their shock-absorbing properties, as well as their easier removal in case of fracture due to their lower friction coefficients [22].
Schwitalla, et al. [23] reported that PEEK screws filled with short carbon fibers (with up to 40% composition) had lower fracture resistance than titanium.
Using an external hexagonal implant and UCLA-type abutment assembly, Neumann, et al. [24] compared the in vitro fracture resistance of implant abutment retention screws made of titanium, PEEK, and 30% carbon fiber-reinforced PEEK. All abutment screws made from the above materials experienced fractures at the neck. Nevertheless, abutment screws made of PEEK and 30% CFR PEEK had lower fracture resistance than titanium.
The future challenge for PEEK abutment screws will be to find the right balance in filler composition in terms of quantity and structure, abutment material and implant connection design. To date, the scientific evidence lacks the consistency needed to recommend their use.
Crowns
The screw-retained implant crown made of PEEK has potential for implant restorations [25]. In addition, due to the high elastic modulus of the metal framework and the mobility of the abutments, resin bonded restorations are subject to unfavorable stress concentrations at the bonded interface; therefore, the risk of debonding might be increased.
Tekin, et al. [26]. Conducted a study to compare the stresses on peri-implant bone, implants, crowns, abutments and screws after loading using PEEK materials. They observed that using PEEK crowns instead of metal ceramic crowns made no significant difference in terms of bone and implant stress. The use of PEEK crowns reduced stresses on themselves and on the abutments. When the PEEK crown was used on titanium abutments, the stress on the screw was reduced and when it was used on a PEEK abutment, the stress increased. It was observed in all tests that the use of PEEK material in this study reduced the stresses resulting from the forces applied to itself.
Because of its low water solubility and low reactivity with other substances, PEEK may also be suitable for patients with metal allergy or metallic taste sensitivity.
Wachtel, et al. [25] conducted a study to evaluate the bacterial seal of PEEK screw-retained crowns on titanium implants with a tapered Implant-Abutment Interface (IAI) during a masticatory simulation and subsequent flexion test. Ten screw-retained upper central incisor implant crowns consisting of a composite-clad PEEK crown framework were connected to NobelActive RP titanium implants (4.3 × 11.5 mm, Nobel Biocare AB, Gothenburg, Sweden) with a tightening torque of 15 Ncm.
Before tightening, the inside of the implant was inoculated with a bacterial suspension of Enterococcus faecium. The specimens were overmolded with an indicator agar that turns black upon contact with E. faecium. During masticatory simulation, no loosening of the implant screws or damage to the veneer or PEEK framework was observed. In addition, no bacterial leakage could be observed in any of the specimens.
Prosthetic applications of peek
Removable dental prostheses: Traditionally, metals (mainly cobalt-chromium [Cr-Co]) are used as framework material for removable dentures. They are still used because of their lower cost [27]. However, these metallic dentures have some disadvantages such as aesthetic unacceptability by the patient, heaviness of the denture and metallic taste, which led to the search for new materials to overcome these disadvantages. PEEK has thus been presented as an alternative framework material to base metal alloys [27,28].
PEEK is a promising alternative material for metal-free removable dental prostheses that has favorable characteristics such as superior mechanical properties, good thermal and chemical resistance, and radiographic transparency [11]. In addition, it can be used to avoid the unpopular silver color and allergies that are commonly seen in conventional metal dentures. In addition, the low modulus of elasticity of PEEK ensures lighter removable dentures and provides a damping effect of occlusal forces [11,29].
Harb, et al. [28] presented a clinical report on the fabrication of the PEEK framework of the Kennedy Class I removable partial denture by CAD/CAM milling technology. They suggested that milled PEEK could be a useful alternative material for the framework of removable partial dentures when restoring edentulous Kennedy Class I patients.
PEEK has good fracture resistance but is mechanically somewhat weak in the homogeneous state. In vitro studies by Tannous, et al. [30] have shown that PEEK clasps have lower strength than cobalt-chromium clasps.
Various studies have compared the reliability of conventional (CoCr) and PEEK materials. In some clinical practices, PEEK has emerged as an esthetic alternative to removable prostheses for CoCr, as the precision of these removable prosthesis frameworks have shown good adaptation [11,28].
Panagiotis Zoidis performed a clinical study on a 70-year-old patient with a conventional distal mandibular extension Cr-Co removable prosthesis. The patient complained about the metallic taste, weight and unpleasant appearance of the metal clasps of her existing Cr-Co prosthesis and requested an alternative material for fabrication of a new prosthesis. He treated the patient with a modified PEEK (Bio-HPP) distal extension framework with acrylic teeth and a conventional thermoset resin prosthetic base [27]. Zoidis performed a 1-year follow-up after the completion of treatment. In his follow-up, he found that there was no breakage of the denture framework and that there was good retention of the clasp and color stability of the Bio-HPP.
Aesthetically, clasps and occlusal cleats made of PEEK provided satisfactory and aesthetically pleasing metal-free results for patients with high aesthetic demands [19].
Temporary fixed dental prostheses
The temporary prosthesis is an intermediate step between the dental preparation and the placement of the final prosthesis. It is used in the short or medium term depending on the clinical situation [31].
In the literature, it has been reported that temporary crowns fabricated using the indirect CAD/CAM technique are stronger and more suitable than conventional temporary crowns fabricated using the direct technique, i.e., chairside without a laboratory step.
Therefore, Abdullah AO, et al. [31] wanted to compare in vitro the average marginal fit, internal fit, fracture resistance and fracture mode of CAD/CAM provisional crowns with direct provisional crowns. The average marginal fit represents the average space between the tooth and the crown at the peripheral joint, while the average internal fit measures the average space between the intrados of the crown and the tooth, in micrometers (μm). Fracture strength is the maximum stress a material will withstand, in Newtons (N), before fracturing. PEEK temporaries demonstrated superior marginal and internal fit in this study compared to temporaries made by direct method, as well as higher fracture resistance.
Bonded temporary bridge: Another interesting application is the use of PEEK as a bonded temporary bridge. Its lower modulus of elasticity than the materials normally used limits the stresses at the bonding interface and thus the risk of delamination. Its low weight and color are also criteria in favor of its use.
Zoidis P, et al. [32] performed a 3-puncture bonded bridge as a temporization prosthesis after placement of 2 implants in the mandibular anterior region. The 52-year-old patient had high mobility of teeth 31, 41 and 42, associated with bone loss. The treatment plan included extraction of these 3 teeth followed by immediate placement of 2 implants with healing screws, and placement of a temporary bridge bonded to 3 pontics during the osseointegration period. The impression was taken 10 days after implant placement using polyvinylsiloxane. The resulting plaster model was scanned with an optical camera, and the bridge framework was designed with CAD/CAM software before being created by PEEK injection molding. After conditioning the outer surface of the PEEK by abrasion, ethanol cleaning and application of adhesive agent, a composite resin coating reproducing the shape of the teeth was light cured. Finally, the bridge was fixed in the mouth with a dual-setting resin cement, i.e., both light-curing and chemically curable (Panavia 21, Kuraray). The patient was instructed to clean the prosthesis daily with a toothbrush and interdental brushes. After 4 months, no detachment or staining was reported.
Permanent fixed dental prostheses
Fixed dental prostheses have long been the gold standard for replacing lost teeth because they improve patient satisfaction, chewing, and comfort [33].
PEEK can be used to fabricate the framework of fixed dentures. It can also be used to prepare dental crowns with a veneer composite facial coating. Therefore, many procedures have been illustrated to facilitate the bonding of PEEK with a resin composite crown. Application of a bonding agent increases the tensile strength of the composite resin. Etching with various acids such as sulfuric acid and piranha acid also increases the bond strength to the resin [27].
A systematic review by Kamlesh, et al. [33] comparing Polyether Ether Ketone (PEEK) to metal-ceramic alloy as a fixed partial denture framework found that fixed partial dentures made of PEEK would have better esthetics, and despite the fact that PEEK frameworks have equivalent mechanical properties to metal alloys, there is not enough evidence to validate superior mechanical properties to metal alloys. Future studies are therefore needed in this area for better understanding and authentication.
CAD/CAM designed PEEK fixed prostheses have superior mechanical properties compared to conventional fixed prostheses according to Reddy, et al. [29] and Stawarczyk, et al. [34]. The fracture resistance of CAD/CAM milled PEEK fixed prostheses (2354N) is much higher than lithium disilicate glass ceramic (950N), alumina (851N), zirconia (981-1331N).
The abrasive properties of PEEK are excellent. Despite significantly low elastic moduli and hardness, the abrasion resistance of PEEK is competitive with metal alloys [29].
A force of 400 N is applied cyclically to the teeth during mastication [35].
Three-unit fixed dentures made of PEEK have shown excellent performance in in vitro studies. No damage occurred to the frameworks and no decay was observed during the extended chewing simulation time used to simulate oral stress conditions equivalent to 5 years of intraoral use. The PEEK restorations far exceeded the fracture strength required to support the masticatory forces assumed for the anterior (300N) and posterior (500-600N) regions. Therefore, PEEK substructures could be used in clinical applications [17].
Given the properties of PEEK (biocompatibility, abrasion resistance almost equal to dentin, damping effect...), this material seems to find its place in patients with parafunctional habits.
Indeed, in patients suffering from bruxism, ceramic restorations are contraindicated because of the risk of abrasion of opposing teeth. PEEK, thanks to its low modulus of elasticity (Young’s modulus), would allow for reduced wear of the enamel of the antagonistic teeth.
Zoidis, et al. [36] presented a case report describing the fabrication of three single crowns for a bruxism patient. The abutment teeth were devitalized and weakened due to loss of tooth structure and thin axial walls. The patient wanted a metal-free restoration. A PEEK framework coupled with an esthetic composite resin superstructure was chosen. This solution allowed for protection of opposing teeth and abutments due to improved impact absorption, as well as ease of intraoral repair in the event of chipping. In patients with parafunctions, PEEK is an attractive alternative to metal-free restorations.
Nazari, et al. compared the fracture resistance of implant-supported fixed dental prostheses with excessive crown height made of zirconia, nickel-chromium (Ni-Cr) alloy, and PEEK materials and concluded that all three-unit implant-supported fixed dental prostheses made of zirconia, metal ceramics, and PEEK materials were effective in resisting biting force and parafunctions [33].
Tekin, et al. [26] compared stresses in the peri-implant bone, implants, crowns, abutments, and screws after loading using PEEK materials, and observed that PEEK material reduced abutment stresses significantly. The results also show that PEEK materials are stronger than titanium abutments.
The load usually incurred by the missing tooth must be transferred through the pontin, connectors and abutment.
Due to its superior mechanical, biological and aesthetic properties, PEEK appears to be a promising alternative to titanium and its alloys. It can be used as a framework material for metal-free fixed dentures, removable dentures, implant-supported fixed dentures, implant-supported overdentures and resin-bonded fixed dentures. It has also been used for the fabrication of dental implants, implant abutments, healing abutments, abutment screws and occlusal splints. Further in vivo research is still needed to determine if PEEK can completely replace titanium and other implant materials in the future.
Ethical approval: This literature review is exempt from ethical approval at our institution.
Author contribution: All authors have contribute to this review.
Provenance and peer review: Not commissioned, externally peer reviewed.
- Blanch-Martínez N, Arias-Herrera S, Martínez-González A. Behavior of polyether-ether-ketone (PEEK) in prostheses on dental implants. A review. J Clin Exp Dent. 2021 May 1;13(5):e520-e526. doi: 10.4317/jced.58102. PMID: 33981401; PMCID: PMC8106930.
- Schwitalla A, Müller WD. PEEK dental implants: a review of the literature. J Oral Implantol. 2013 Dec;39(6):743-9. doi: 10.1563/AAID-JOI-D-11-00002. Epub 2011 Sep 9. PMID: 21905892.
- Saxena D, Varshney N, Tomar S, Rawat P. THE SCOPE OF PEEK IN DENTAL IMPLANTOLOGY: LITERATURE REVIEW. Journal of Pharmaceutical Negative Results. 2022; 3472‑5.
- Kanchanasobhana C, Suphangul S, Rungsiyakull P, Chaijareenont P. PEEK Material in Terms of Biomechanics and its use in Single Implant Prosthesis: A Review. J. Int Dent Med Res. 2022; 15(4): 1753-1762.
- Kumar B, Ramajayam S. Peek in dental implant-A review of literature. World Journal of Advanced Research and Reviews. 2022; 15(2):139‑143.
- Skirbutis G, Dzingutė A, Masiliūnaitė V, Šulcaitė G, Žilinskas J. A review of PEEK polymer's properties and its use in prosthodontics. Stomatologija. 2017;19(1):19-23. PMID: 29243680.
- Yin W, Chen M, Bai J, Xu Y, Wang M, Geng D. Recent advances in orthopedic polyetheretherketone biomaterials: Material fabrication and biofunction establishment. Smart Materials in Medicine. 2022; 3:20‑36.
- Elawadly T, Radi IAW, El Khadem A, Osman RB. Can PEEK Be an Implant Material? Evaluation of Surface Topography and Wettability of Filled Versus Unfilled PEEK With Different Surface Roughness. J Oral Implantol. 2017 Dec;43(6):456-461. doi: 10.1563/aaid-joi-D-17-00144. Epub 2017 Oct 24. PMID: 29064768.
- Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthodont Res. 2016 Jan;60(1):12-9. doi: 10.1016/j.jpor.2015.10.001. PMID: 26520679.
- Meningaud JP, Spahn F, Donsimoni JM. L'après titane, le PEEK? [After titanium, peek ?]. Rev Stomatol Chir Maxillofac. 2012 Nov;113(5):407-10. French. doi: 10.1016/j.stomax.2011.12.016. Epub 2012 Aug 30. PMID: 22940377.
- Liu Y, Fang M, Zhao R, Liu H, Li K, Tian M, Niu L, Xie R, Bai S. Clinical Applications of Polyetheretherketone in Removable Dental Prostheses: Accuracy, Characteristics, and Performance. Polymers (Basel). 2022 Oct 31;14(21):4615. doi: 10.3390/polym14214615. PMID: 36365609; PMCID: PMC9654455.
- Barkarmo S, Longhorn D, Leer K, Johansson CB, Stenport V, Franco-Tabares S, Kuehne SA, Sammons R. Biofilm formation on polyetheretherketone and titanium surfaces. Clin Exp Dent Res. 2019 Jun 13;5(4):427-437. doi: 10.1002/cre2.205. PMID: 31452954; PMCID: PMC6704035.
- D'Ercole S, Cellini L, Pilato S, Di Lodovico S, Iezzi G, Piattelli A, Petrini M. Material characterization and Streptococcus oralis adhesion on Polyetheretherketone (PEEK) and titanium surfaces used in implantology. J Mater Sci Mater Med. 2020 Sep 28;31(10):84. doi: 10.1007/s10856-020-06408-3. PMID: 32989624; PMCID: PMC7522102.
- Rahmitasari F, Ishida Y, Kurahashi K, Matsuda T, Watanabe M, Ichikawa T. PEEK with Reinforced Materials and Modifications for Dental Implant Applications. Dent J (Basel). 2017 Dec 15;5(4):35. doi: 10.3390/dj5040035. PMID: 29563441; PMCID: PMC5806965.
- Russel ME, Madhu S. A Review on The Tribological Behavior of Polyether Ether Ketone (PEEK). Annals of the Romanian Society for Cell Biology. 2021; 20312‑21.
- Liebermann A, Wimmer T, Schmidlin PR, Scherer H, Löffler P, Roos M, Stawarczyk B. Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/CAM polymers after aging in different storage media. J Prosthet Dent. 2016 Mar;115(3):321-8.e2. doi: 10.1016/j.prosdent.2015.09.004. Epub 2015 Nov 6. PMID: 26548869.
- Tabasum S, Shetty P, Goutam M. Sneak peek into peek polymer: An Innovation. Journal Of Applied Dental and Medical Sciences. 2018; 4:1.
- Santing HJ, Meijer HJ, Raghoebar GM, Özcan M. Fracture strength and failure mode of maxillary implant-supported provisional single crowns: a comparison of composite resin crowns fabricated directly over PEEK abutments and solid titanium abutments. Clin Implant Dent Relat Res. 2012 Dec;14(6):882-9. doi: 10.1111/j.1708-8208.2010.00322.x. Epub 2010 Dec 22. PMID: 21176099.
- Qin L, Yao S, Zhao J, Zhou C, Oates TW, Weir MD, Wu J, Xu HHK. Review on Development and Dental Applications of Polyetheretherketone-Based Biomaterials and Restorations. Materials (Basel). 2021 Jan 15;14(2):408. doi: 10.3390/ma14020408. PMID: 33467576; PMCID: PMC7830426.
- Mishra S, Chowdhary R. PEEK materials as an alternative to titanium in dental implants: A systematic review. Clinical implant dentistry and related research. 2019; 21(1):208‑22.
- Ortega-Martínez J, Delgado LM, Ortiz-Hernández M, Punset M, Cano-Batalla J, Cayon MR, Cabratosa-Termes J. In vitro assessment of PEEK and titanium implant abutments: Screw loosening and microleakage evaluations under dynamic mechanical testing. J Prosthet Dent. 2022 Mar;127(3):470-476. doi: 10.1016/j.prosdent.2020.09.033. Epub 2020 Dec 9. PMID: 33309211.
- Paratelli A, Perrone G, Ortega R, Gómez-Polo M. Polyetheretherketone in Implant Prosthodontics: A Scoping Review. Int J Prosthodont. 2020 Nov/Dec;33(6):671-679. doi: 10.11607/ijp.6649. PMID: 33284910.
- Schwitalla AD, Abou-Emara M, Zimmermann T, Spintig T, Beuer F, Lackmann J, Müller WD. The applicability of PEEK-based abutment screws. J Mech Behav Biomed Mater. 2016 Oct;63:244-251. doi: 10.1016/j.jmbbm.2016.06.024. Epub 2016 Jul 1. PMID: 27434650.
- Neumann EA, Villar CC, França FM. Fracture resistance of abutment screws made of titanium, polyetheretherketone, and carbon fiber-reinforced polyetheretherketone. Braz Oral Res. 2014;28:S1806-83242014000100239. doi: 10.1590/1807-3107bor-2014.vol28.0028. Epub 2014 Aug 4. PMID: 25098826.
- Wachtel A, Zimmermann T, Sütel M, Adali U, Abou-Emara M, Müller WD, Mühlemann S, Schwitalla AD. Bacterial leakage and bending moments of screw-retained, composite-veneered PEEK implant crowns. J Mech Behav Biomed Mater. 2019 Mar;91:32-37. doi: 10.1016/j.jmbbm.2018.11.027. Epub 2018 Nov 28. PMID: 30529984.
- Tekin S, Değer Y, Demirci F. Evaluation of the use of PEEK material in implant-supported fixed restorations by finite element analysis. Niger J Clin Pract. 2019 Sep;22(9):1252-1258. doi: 10.4103/njcp.njcp_144_19. PMID: 31489862.
- Pai SA, Kumari S, Umamaheswari B, Jyothi M, Lakshmi CS. Polyetheretherketone in prosthodontics–A review. Journal of Advanced Clinical and Research Insights. 2019; 6(1):24‑6.
- Harb IE, Abdel-Khalek EA, Hegazy SA. CAD/CAM Constructed Poly(etheretherketone) (PEEK) Framework of Kennedy Class I Removable Partial Denture: A Clinical Report. J Prosthodont. 2019 Feb;28(2):e595-e598. doi: 10.1111/jopr.12968. Epub 2018 Oct 21. PMID: 30345575.
- Reddy MST, Velayudhan A, Ganapathy D, Venugopalan S, Neppala G. A Peek into PEEK: the trending dental biomaterial-A Review. Journal of Pharmaceutical Negative Results. 2022; 396‑402.
- Tannous F, Steiner M, Shahin R, Kern M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent Mater. 2012 Mar;28(3):273-8. doi: 10.1016/j.dental.2011.10.016. Epub 2011 Nov 29. PMID: 22130464.
- Abdullah AO, Tsitrou EA, Pollington S. Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns. J Appl Oral Sci. 2016 May-Jun;24(3):258-63. doi: 10.1590/1678-775720150451. PMID: 27383707; PMCID: PMC5022219.
- Zoidis P, Papathanasiou I. Modified PEEK resin-bonded fixed dental prosthesis as an interim restoration after implant placement. J Prosthet Dent. 2016 Nov;116(5):637-641. doi: 10.1016/j.prosdent.2016.04.024. Epub 2016 Jul 28. PMID: 27475921.
- Kamlesh RD, Nallaswamy D, Ganapathy D. Effectiveness of PEEK Framework in Comparison to Metal Framework for Fixed Dental Prosthesis: A Systematic Review. J Dent. 2022; 13(1):80‑6.
- Stawarczyk B, Beuer F, Wimmer T, Jahn D, Sener B, Roos M, Schmidlin PR. Polyetheretherketone-a suitable material for fixed dental prostheses? J Biomed Mater Res B Appl Biomater. 2013 Oct;101(7):1209-16. doi: 10.1002/jbm.b.32932. Epub 2013 Apr 6. PMID: 23564476.
- Bhargav A, Malhotra P, Giri S, Kaur P, Lall AB, Nautiyal A. Characteristics of Peek Polymer and Its Application in Dentistry: A Review.
- Zoidis P, Bakiri E, Papathanasiou I, Zappi A. Modified PEEK as an alternative crown framework material for weak abutment teeth: a case report. Gen Dent. 2017 Sep-Oct;65(5):37-40. PMID: 28862587.